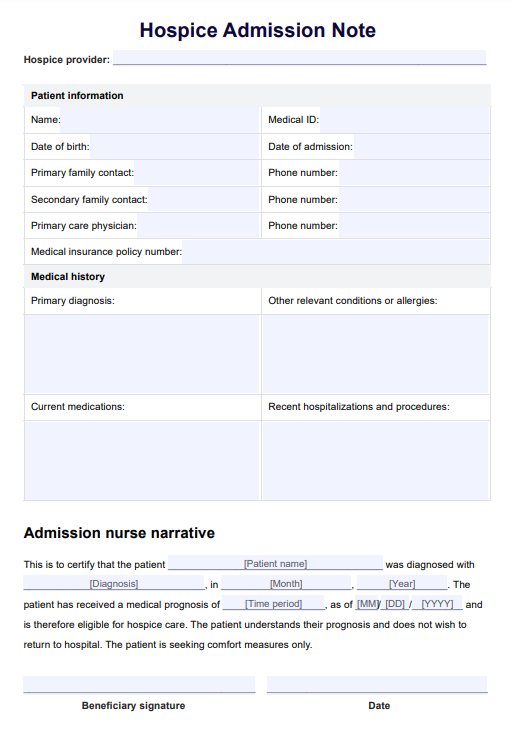
A hospice admissions note typically includes essential patient details, such as demographic information, medical history, current diagnoses, medications, end-of-life care preferences, consent, insurance information, and acknowledgments of hospice program policies.
Hospice Admission Note Template
Streamline the admission process with our Hospice Admission Note Template and provide compassionate end-of-life care.
Hospice Admission Note Template Template
Commonly asked questions
Healthcare professionals will complete hospice admission notes upon patients' admission to the hospice program. Interdisciplinary team members (hospice nurses, physicians, or social workers) gather and document the necessary information during admission.
Yes, modifications or additions to the hospice admission note can be made if necessary. To ensure the accuracy and completeness of the information, any changes or updates in the patient's condition, care preferences, or legal documents can be made by amending hospice documentation.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











