Marfan syndrome is diagnosed through a combination of a detailed medical history, physical examination, genetic testing, and imaging tests like echocardiograms to check for features of the condition.
Improve diagnoses and care for patients with Marfan syndrome using our Marfan Syndrome Diagnosis Criteria.
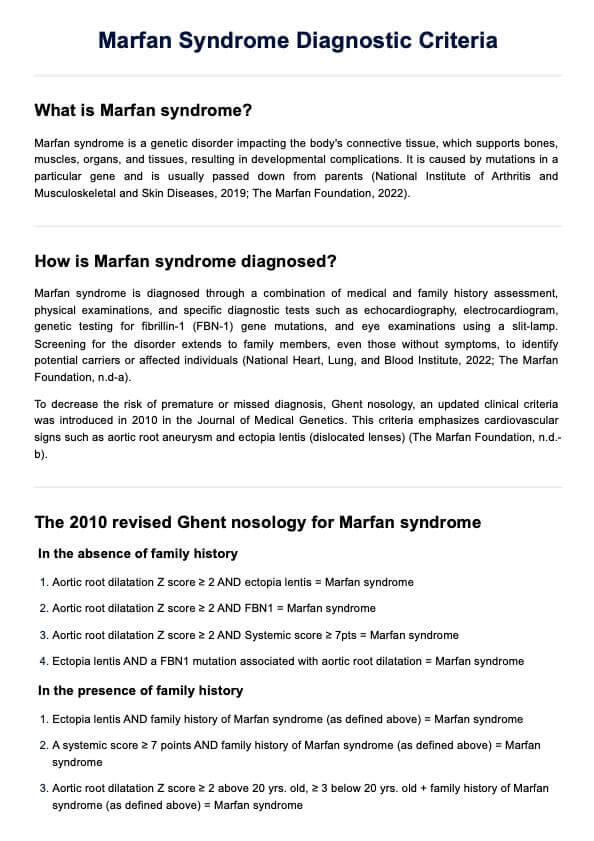
Marfan syndrome is diagnosed through a combination of a detailed medical history, physical examination, genetic testing, and imaging tests like echocardiograms to check for features of the condition.
Before proper interventions and surgical procedures were available, the life expectancy for people with Marfan syndrome was 30-40 years, but with modern medical care and regular monitoring, it can extend to 70 years or more.
Marfan syndrome can appear at any age, with some symptoms present at birth and others developing later in childhood, adolescence, or adulthood.
EHR and practice management software
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments