Clinical notes encompass a broad spectrum of location details of patient encounters, including assessments, diagnoses, treatments, and progress notes. They document ongoing patient care, medical history, and treatment plans. On the other hand, procedure notes detail the specifics of medical procedures or interventions performed on a patient.
Procedure Note Template
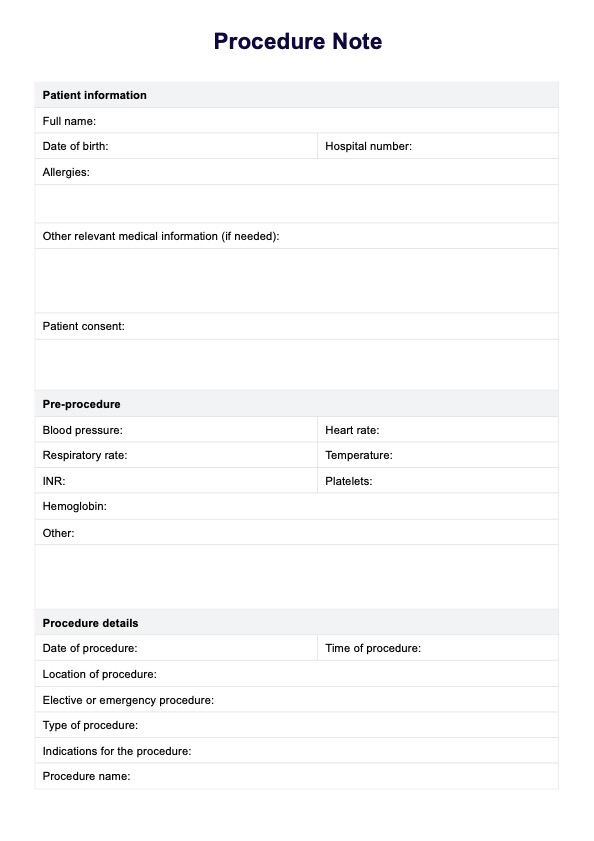
Ensure patient identity, consent, anesthesia, vital signs, and complications are documented. Download our accessible Procedure Note Template today!
Procedure Note Template Template
Commonly asked questions
To create procedure notes on Carepatron, navigate to the documentation section of the software and select the option to make a new procedure note. Input the relevant details of the procedure, including patient identification, consent, anesthesia administration, vital signs, and any complications encountered. Utilize the provided templates or customize the format to suit your practice's needs.
A comprehensive procedure note should capture critical details of the medical intervention. This typically includes verifying patient identity, documenting informed consent, and recording vital signs. Details about anesthesia, foreign body bodies encountered, and the procedure are also important. These requirements may vary depending on the specific procedure.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











