It serves as a legal record of the care provided and hospice eligibility, ensuring compliance with regulatory standards. Additionally, comprehensive documentation supports continuity of care by providing a clear and detailed history of the patient's condition and the interventions undertaken.
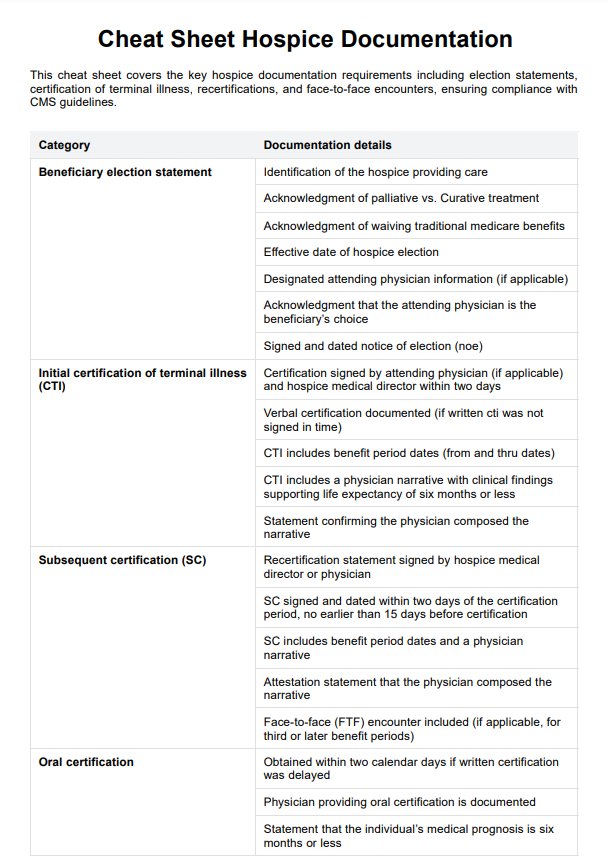
Cheat Sheet Hospice Documentation Template
Comprehensive guide to hospice documentation: ensure quality care, regulatory compliance, and effective interdisciplinary communication. Streamline your process with expert tips.
Cheat Sheet Hospice Documentation Template Template
Commonly asked questions
Documentation for pain management in hospice care should include the patient's self-reported pain levels, the effectiveness of prescribed medications, and any non-pharmacological interventions used.
Documenting emotional and spiritual support in hospice care involves recording interventions to address the psychosocial and spiritual aspects of the patient's well-being. This includes documenting conversations about the patient's emotional state, any counseling or therapeutic interventions provided, and support for the patient's family.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











