The exact information that you include in your therapist note will depend on the type of session that you have with your client. When you are writing your notes, you may choose to use a specific structure (e.g. SOAP, DAP, or BIRP). However, writing them without a predetermined format is just as acceptable. Under HIPAA guidelines, the type of information that you include in a therapy note differs from that of a progress note. It includes details concerning a conversation you have had with a patient (and this could be a session, a phone call, or another type of encounter). It’s important that you don’t include information regarding diagnosis, symptoms, clinical test results, and treatment plans - otherwise the document will be considered a progress note.
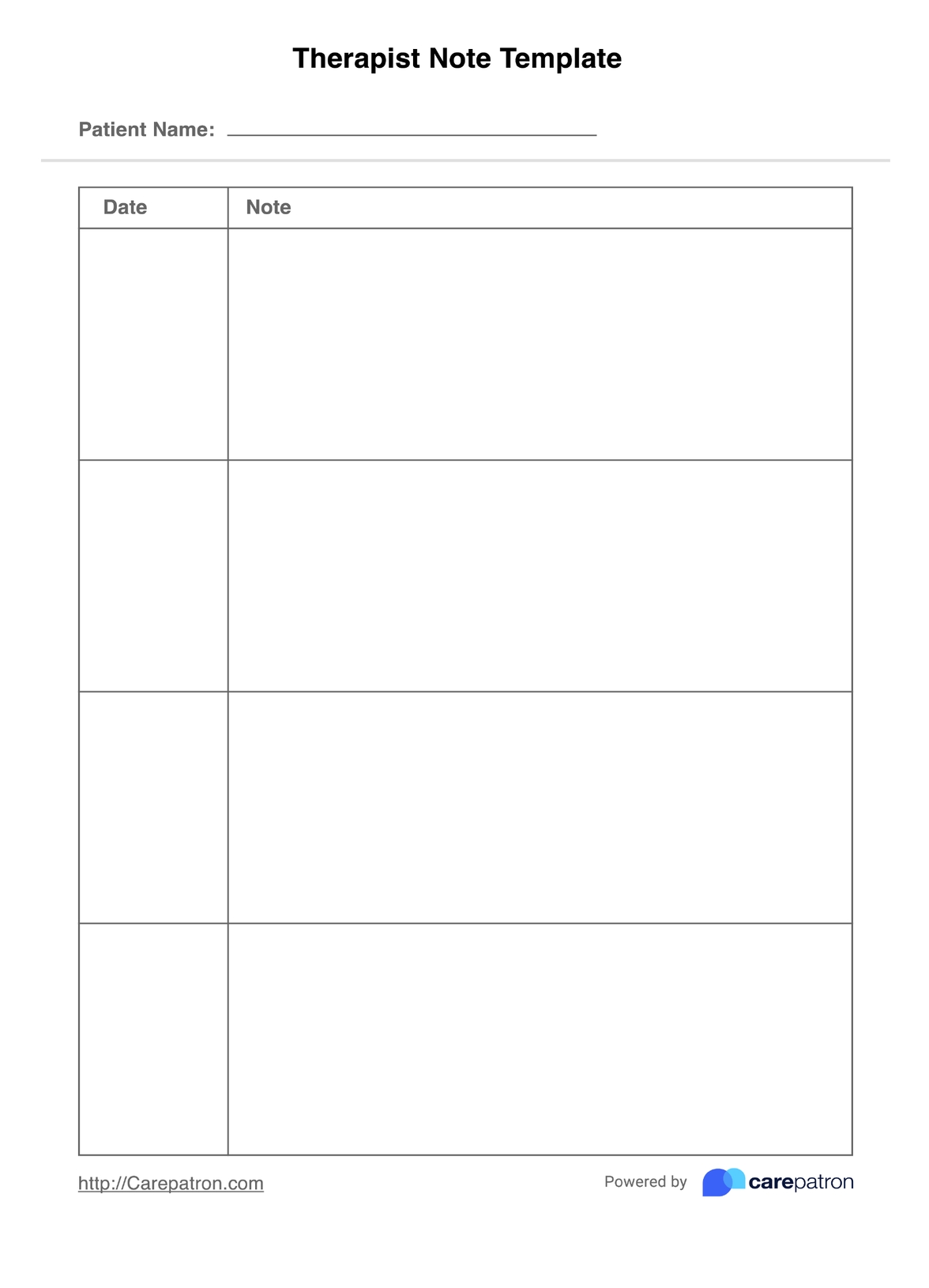
Therapist Notes Template
A simplified therapist note template is guaranteed to help therapists promptly produce comprehensive, detailed, and accurate documents.
Therapist Notes Template Template
Commonly asked questions
Therapy notes are not legal documents, which means that therapists are not required to grant viewing access to their patients. However, patients are allowed to request access, and therapists can decide whether to approve this or not.
The timeliness of writing therapy notes is important. You don’t want to be writing too much during the session with the patient, otherwise, it may seem as though you are distracted. On the other hand, if you wait too long you may forget important details. The best option is to write your therapy notes immediately after each session with a patient.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











