DAP in case management refers to a structured note-taking format used by healthcare professionals, particularly in behavioral health, that stands for Data, Assessment, and Plan. This method helps clinicians document client progress and important session details clearly and concisely, facilitating effective communication among providers and ensuring compliance with record-keeping standards.
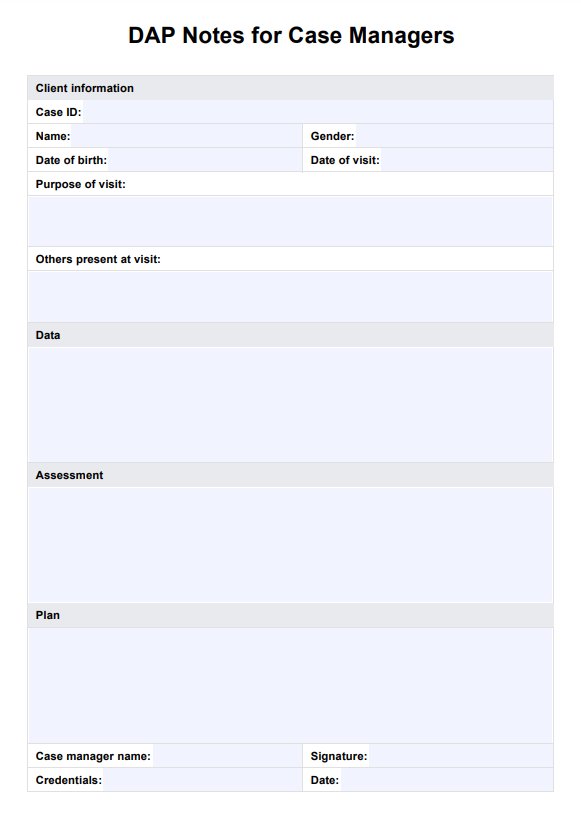
DAP Notes for Case Managers
Master the DAP note format with our free template to streamline your case management process.
DAP Notes for Case Managers Template
Commonly asked questions
The primary difference between SOAP notes and DAP notes lies in their structure: SOAP notes include four components—Subjective, Objective, Assessment, and Plan—while DAP notes streamline this into three sections, focusing on factual data, clinical assessment, and future planning. DAP notes are often preferred in behavioral health settings for their simplicity and directness.
To write DAP notes effectively, begin with the Data section by documenting observable facts and client statements. Next, analyze this information in the Assessment section, interpreting the data to identify symptoms or diagnoses. Finally, outline the Plan, detailing the next steps for treatment or interventions based on the assessment.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











