To write a nursing care plan for meningitis, first assess the patient's condition through comprehensive physical examinations and diagnostic evaluations. Identify nursing diagnoses based on the assessment. Set specific, measurable goals, develop interventions and evaluate the patient's progress towards the goals and adjust the care plan as necessary.
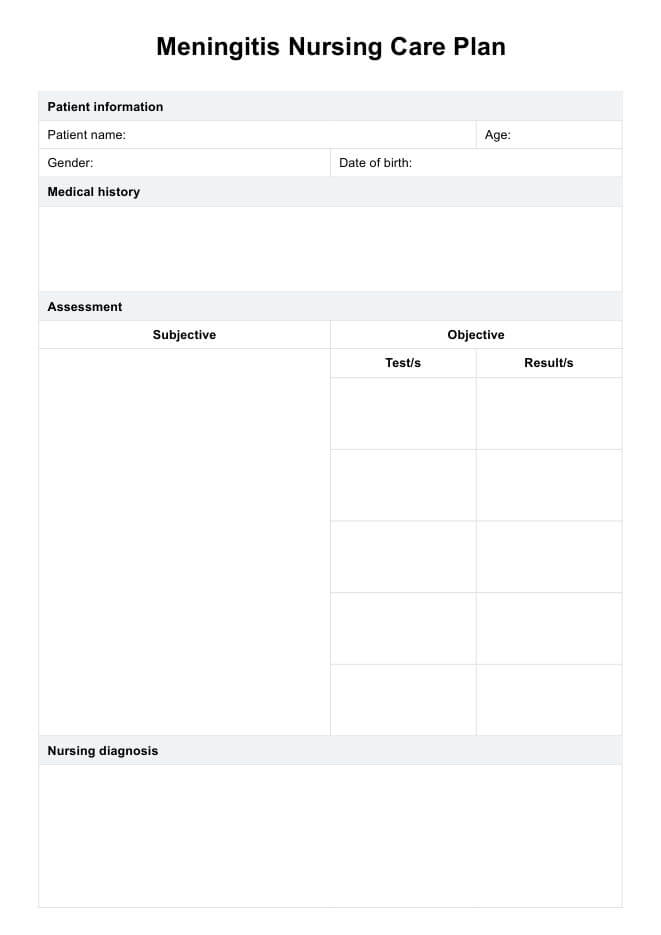
Meningitis Nursing Care Plan
Access Carepatron's free PDF download of a Meningitis Nursing Care Plan and example to help with a nursing diagnosis for meningitis. Learn how to create an effective care plan for patients with meningitis.
Meningitis Nursing Care Plan Template
Commonly asked questions
The primary goal of care for meningitis patients is to promptly identify and treat the underlying infection to prevent complications and promote recovery. Ultimately, the goal is to restore the patient's health and minimize the long-term effects of the illness.
Other conditions that present with similar symptoms, such as viral encephalitis, brain abscess, and migraines, can be differential diagnoses of meningitis. Differentiating between these conditions may require further diagnostic tests and clinical evaluation.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











