The Dialysis Care Plan meeting is a collaborative discussion among healthcare professionals to review and update the care plan for a patient undergoing dialysis. It typically involves nurses, nephrologists, dietitians, and other members of the healthcare team to ensure comprehensive and coordinated care.
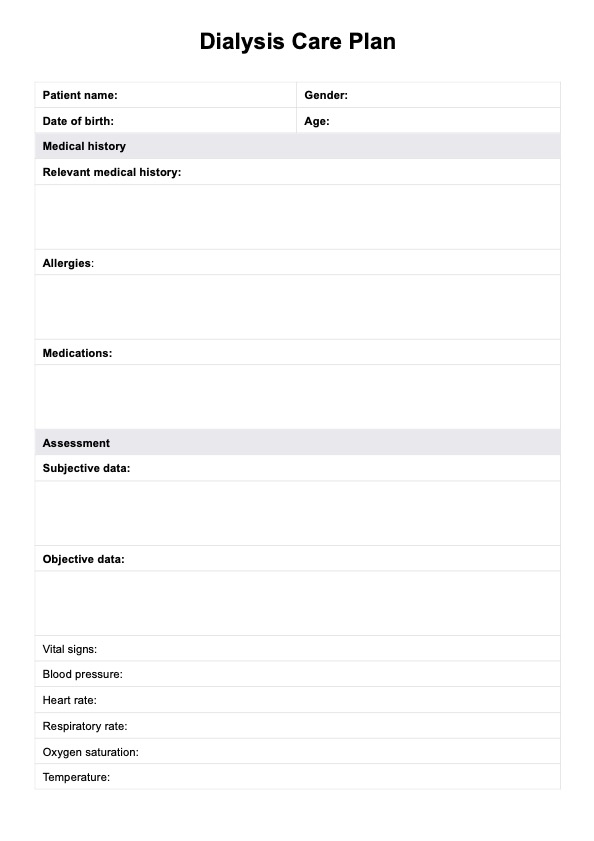
Dialysis Care Plan
Streamline patient care and enhance outcomes with our Dialysis Care Plan template.
Dialysis Care Plan Template
Commonly asked questions
Taking care of a dialysis patient involves monitoring vital signs, assessing vascular access, ensuring adherence to fluid and dietary restrictions, and providing emotional support. It also includes educating patients and their families about the importance of medication adherence and lifestyle modifications.
Nursing assessments after dialysis include monitoring vital signs, assessing vascular access for signs of infection or complications, evaluating fluid status, and observing for any adverse reactions to treatment. Nurses also assess the patient's overall well-being and address any concerns or symptoms that arise post-dialysis.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments