The general principles include thoroughly assessing pain, using a multimodal approach, prescribing the lowest effective dose of pain medications, and regularly monitoring and adjusting treatments.
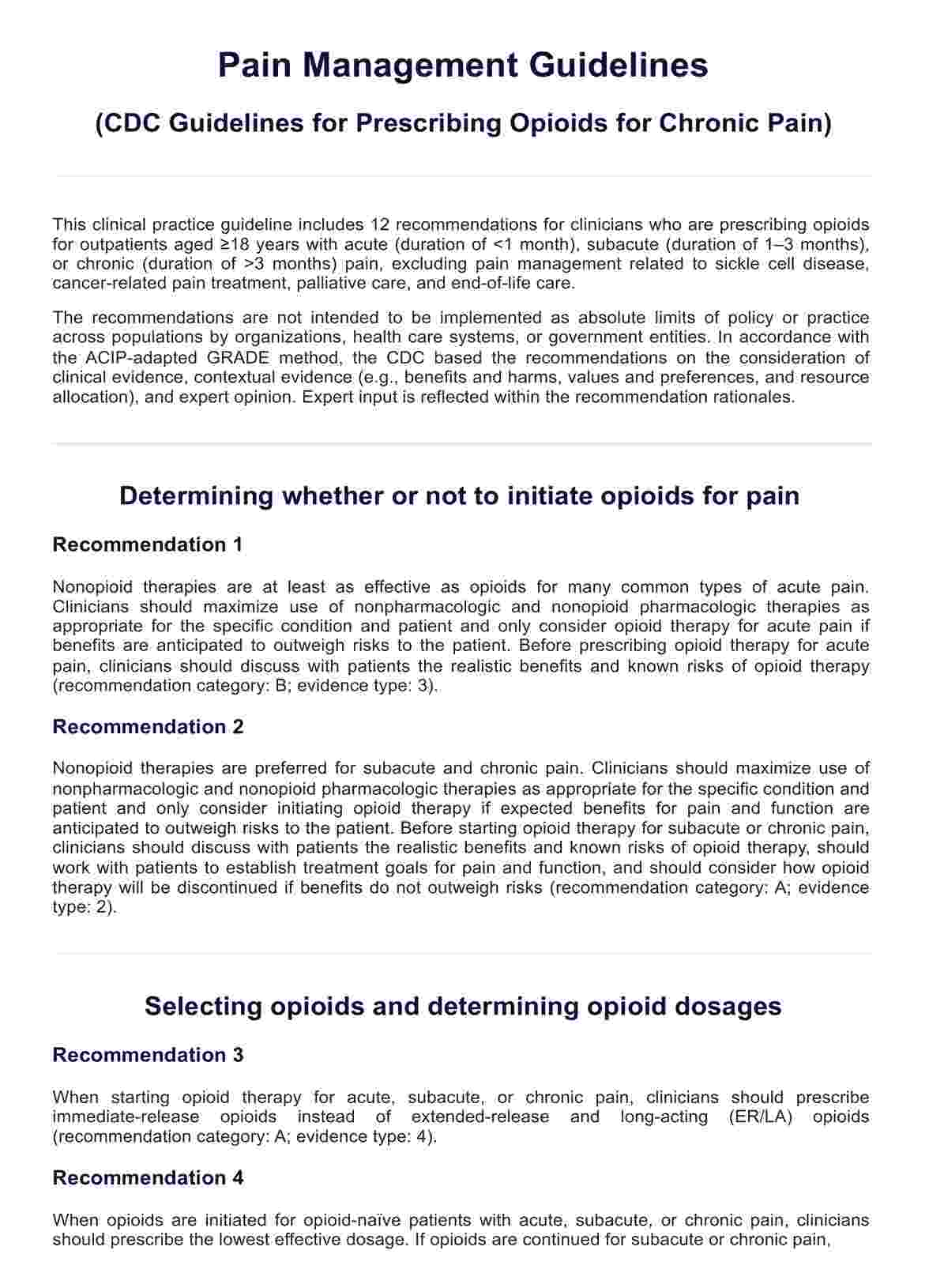
Pain Management Guidelines (CDC Guideline for Prescribing Opioids for Chronic Pain)
Discover evidence-based Pain Management Guidelines designed to enhance patient care. Learn strategies for effectively diagnosing, treating, and managing acute and chronic pain.
Use Template
Pain Management Guidelines (CDC Guideline for Prescribing Opioids for Chronic Pain) Template
Commonly asked questions
Common strategies include medication (opioid and non-opioid), physical therapy, cognitive-behavioral therapy (CBT), acupuncture, and lifestyle modifications like exercise and stress management.
Pain management plans provide structured, individualized treatment approaches that can improve pain control, enhance function, and improve quality of life for those with chronic pain.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











