Assessment for impaired urinary elimination requires a comprehensive evaluation that includes both subjective and objective data. Key findings may include patient-reported symptoms such as urgency, frequency, nocturia, or incontinence, alongside physical examination results like distended bladder or changes in skin integrity. Additionally, laboratory tests (e.g., urinalysis) can provide insight into possible infections or metabolic issues. A thorough understanding of the patient’s medical history and medication use is also crucial in identifying contributing factors.
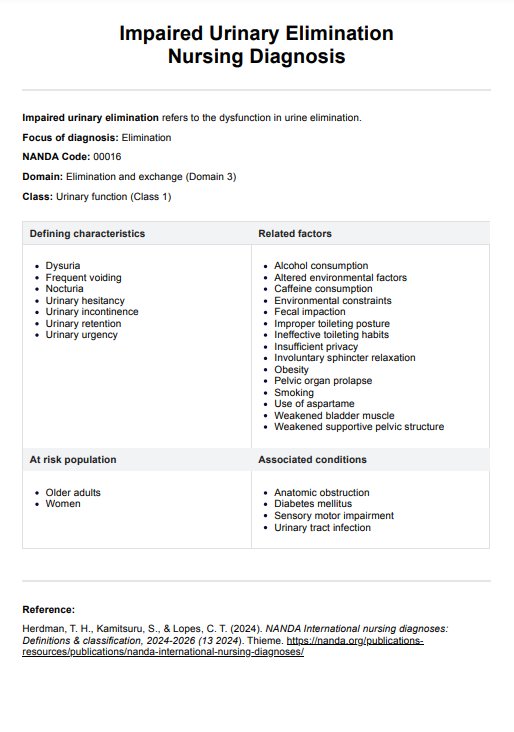
Impaired Urinary Elimination Nursing Diagnosis
Explore essential insights and effective strategies for managing Impaired Urinary Elimination Nursing Diagnosis to enhance patient care and improve outcomes.
Impaired Urinary Elimination Nursing Diagnosis Template
Commonly asked questions
Effective nursing interventions for managing impaired urinary elimination may involve both direct and indirect strategies. First, promoting regular toileting schedules can help reduce incontinence episodes. For patients with cognitive impairments, providing reminders or cues can enhance their ability to recognize the need to void. Implementing pelvic floor muscle training or bladder training programs can also be beneficial. Additionally, ensuring adequate fluid intake and assessing the patient's medications for potential side effects that contribute to urinary issues is essential. Collaborating with interdisciplinary teams, including urologists or physical therapists, may further enhance the management plan.
Evaluating the effectiveness of nursing interventions for impaired urinary elimination requires continuous monitoring and reassessment of the patient's condition. This involves tracking the frequency and characteristics of urinary episodes, assessing patient-reported outcomes related to comfort and confidence, and observing any changes in physical examination findings, such as bladder ditension. Documenting these findings allows for clear communication among healthcare providers and aids in adjusting care plans as necessary.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











