There is no single correct technique to create patient notes. When it comes to patient notes and what should be included, every healthcare practitioner will have a different opinion, so do what works best for you. Keep in mind that it’s quality over quantity and that your notes should be clear, relevant, concise, and include all significant supporting evidence to aid in effective treatment.
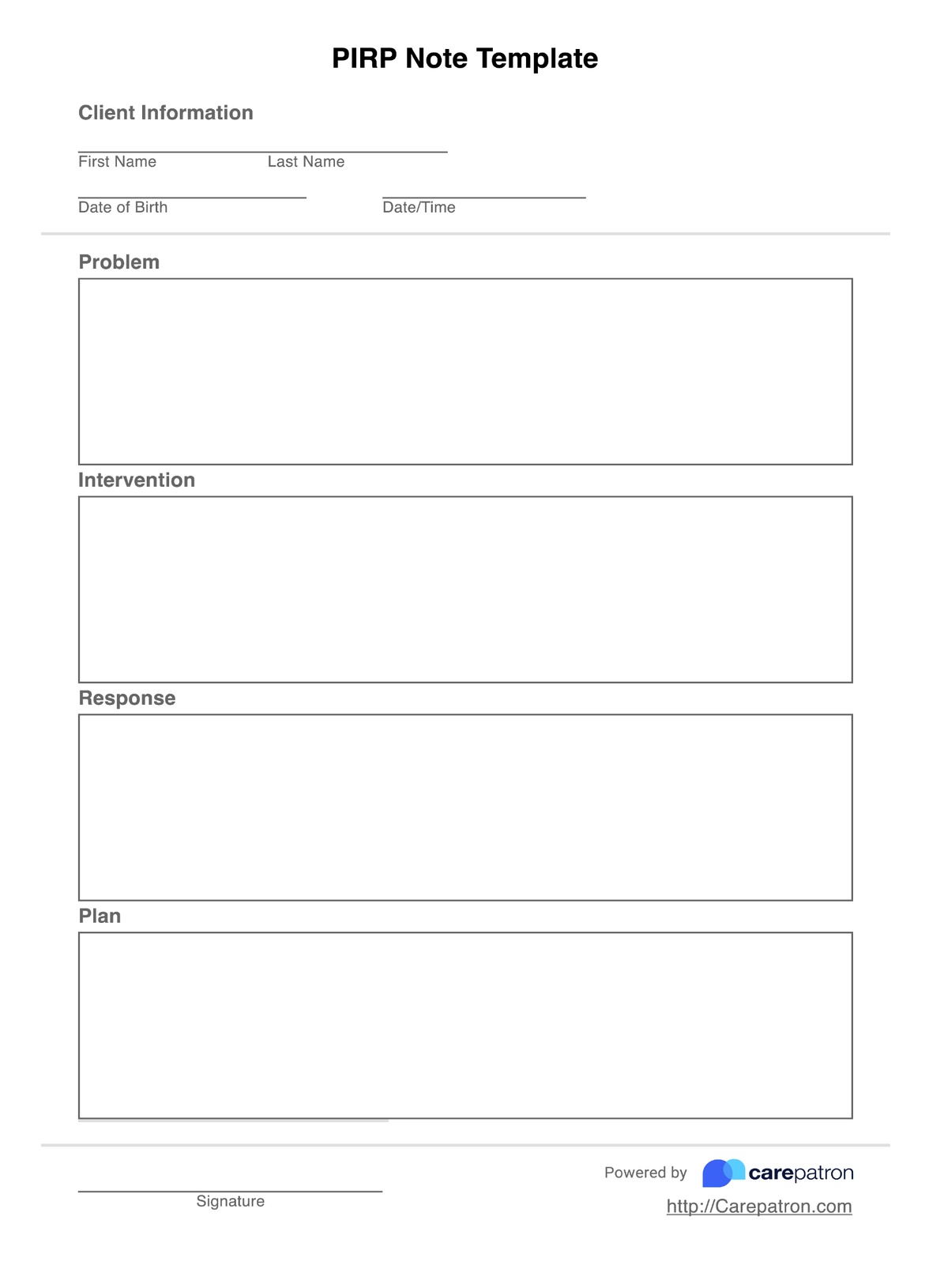
PIRP Notes Template
This high-quality PIRP note template will boost the standard of care in your clinician practice by improving clinical outcomes and developing a more streamlined workflow.
PIRP Notes Template Template
Commonly asked questions
Both progress note formats are excellent, and there is no one method vastly better than the other. It helps to take some time to evaluate what you’re wanting to achieve, and how these formats both contribute to your desired outcome. For example, SOAP is useful for having distinct subjective and objective sections to distill client conditions into specific details, with assessments working to encourage certain interventions. Whereas, PIRP is problem-oriented, considers a broader overlook in terms of a condition in general, and provides on-the-spot intervention introspection.
This can differ from practitioner to practitioner, however, as a general rule, PIRP notes should be 1-2 pages in length. Anything beyond this becomes excessive, and it’s best to keep things short and sweet. Having simple and concise notes means they can be understood by a wider range of people, which is always a plus.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











