The Guided Notes Template is essential because it helps students focus, understand key concepts, and organize information during lessons.
Guided Notes Template
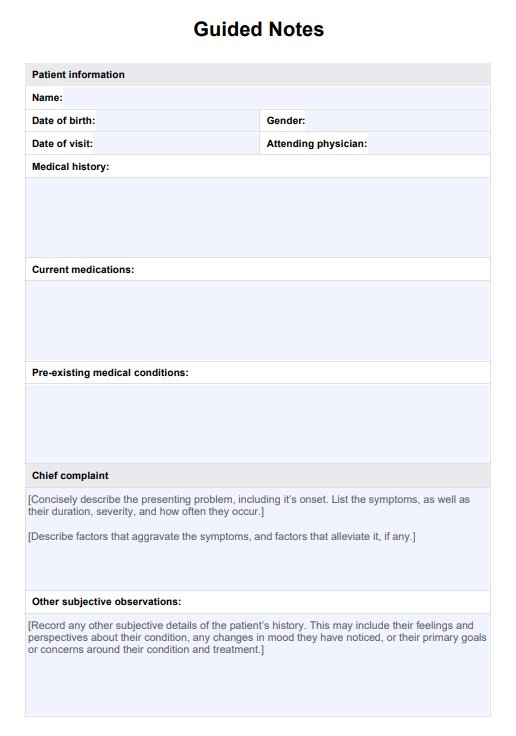
Enhance student learning of clinical documentation skills with our Guided Notes Template, a structured format for compiling comprehensive patient records.
Use Template
Guided Notes Template Template
Commonly asked questions
The guided notes note-taking method is a structured approach where key points or questions are provided in advance, guiding students or learners to focus on essential information during lectures or readings.
To structure guided notes, organize information into sections such as objectives, key concepts, summaries, and questions. Use bullet points or fill-in-the-blank formats to prompt engagement and comprehension.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











