This will depend on the psychiatrist and the type of note they are writing. The note should include the patient’s identifying information to ensure it is assigned to the correct patient and a concise summary of the patient’s updates. The note may also include the patient’s medication regimen, changes to their medication, and the next steps for the patient’s treatment.
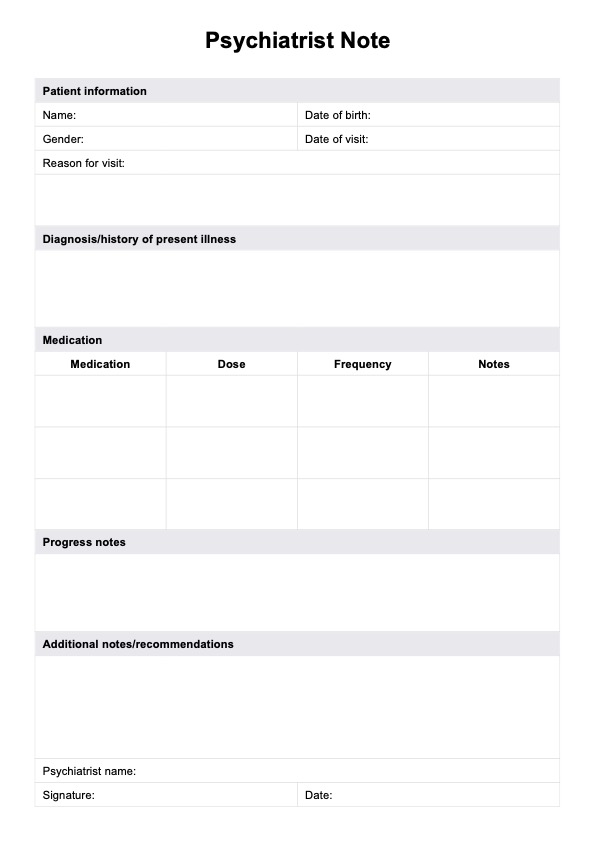
Psychiatrist Note Template
Take concise, comprehensive psychiatric notes using our pre-formatted and structured Psychiatrist Note Template.
Psychiatrist Note Template Template
Commonly asked questions
To write a good psychiatry note, clinicians should ensure it is clear, concise, and comprehensive. The note should include the patient's identifying information, the visit date, and a detailed account of the patient's presenting issues and history. Documenting treatment plans, medication adjustments, and any patient progress or challenges is essential. Maintaining a professional tone and adhering to confidentiality guidelines are crucial for effective communication and legal compliance.
A psych SOAP note follows the structured format of Subjective, Objective, Assessment, and Plan. In the Subjective section, document the patient's self-reported symptoms and concerns. The Objective section should include observable data such as vital signs and mental status exam findings. In the Assessment section, provide your clinical interpretation of the information gathered, including diagnoses or changes in condition. Finally, outline a clear Plan that details treatment interventions, follow-up appointments, and any referrals needed.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











