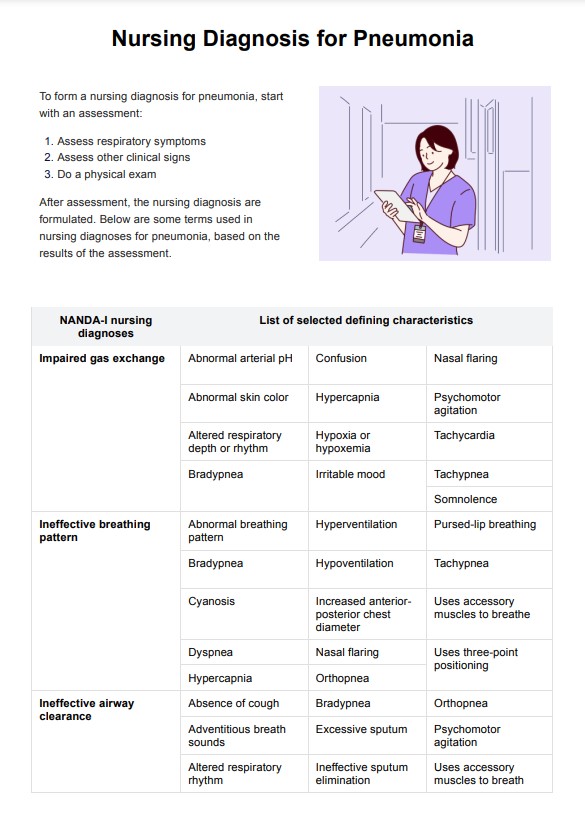
A NANDA nursing diagnosis for respiratory patients is a standardized statement that identifies specific health issues related to respiratory function. Examples include "Impaired gas exchange related to alveolar-capillary membrane changes" and "Ineffective airway clearance related to increased sputum production."
Nursing Diagnosis for Pneumonia
Explore our guide on pneumonia, including symptoms, treatments, and how our free template can help form accurate nursing diagnoses.
Nursing Diagnosis for Pneumonia Template
Commonly asked questions
Nurses assess respiratory status, administer medications, provide supplemental oxygen or do oxygen therapy, and educate patients on breathing exercises and infection prevention. They also monitor vital signs, ensure adequate hydration, and support patients in managing symptoms like cough and fever.
The primary goals of care for pneumonia are to clear the infection, improve gas exchange, manage symptoms, prevent complications, and promote recovery. This involves reducing inflammation, maintaining oxygenation, and ensuring patient comfort.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











