Osteomyelitis can be classified into acute, chronic, and subacute forms based on the duration and severity of the infection.
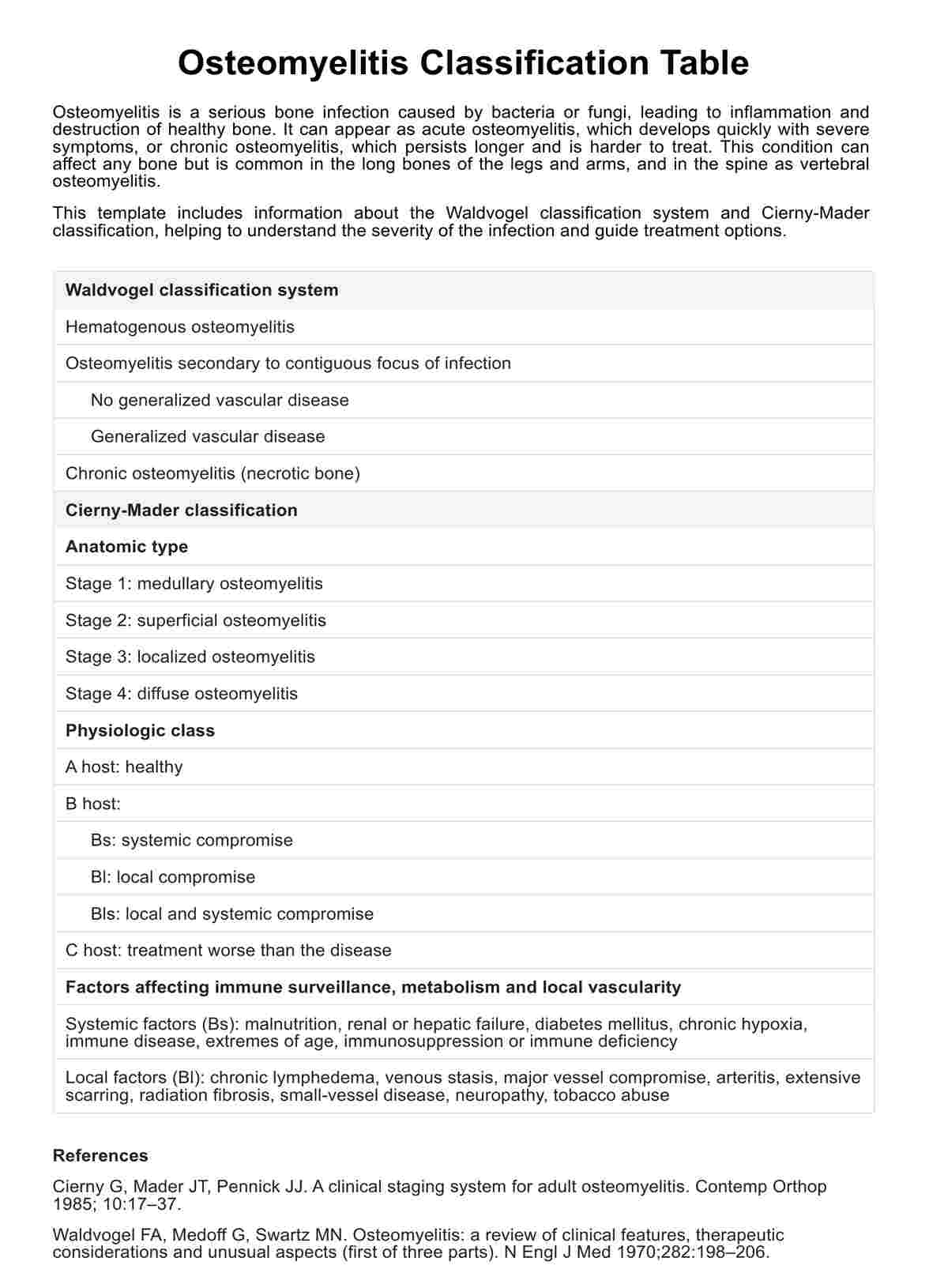
Osteomyelitis Classification Table
Get Carepatron's free PDF download of an Osteomyelitis Classification Table along with examples for easy reference and understanding of this medical condition.
Use Template
Osteomyelitis Classification Table Template
Commonly asked questions
Osteomyelitis is a bone infection characterized by inflammation and destruction of bone tissue, often caused by bacterial or fungal pathogens.
The main cause of osteomyelitis is bacterial infection, with Staphylococcus aureus being the most common pathogen involved.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











