Developing a nursing care plan for fluid retention and electrolyte imbalance can take anywhere from 30 minutes to several hours, depending on the complexity of the patient's condition, required assessments, and individualized interventions.
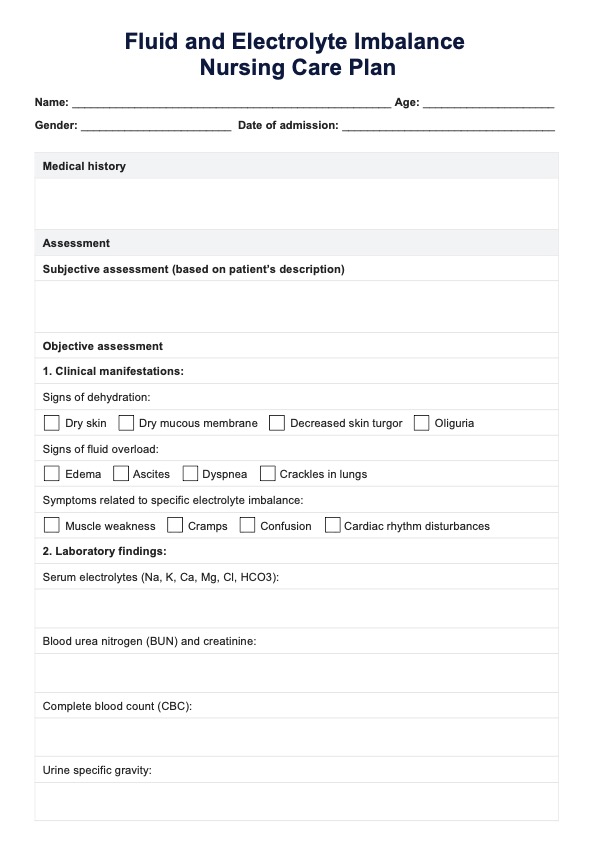
Fluid and Electrolyte Imbalance Nursing Care Plan
Discover key strategies for managing fluid intake, electrolyte balance, and nursing interventions for imbalances. Download the PDF guide now!
Fluid and Electrolyte Imbalance Nursing Care Plan Template
Commonly asked questions
You can monitor fluid intake by accurately tracking oral and intravenous fluids administered. Document all intake amounts, assess urine output and adjust the care plan based on changes in fluid balance and vital signs.
Common signs and symptoms of electrolyte imbalances include muscle weakness, cramps, fatigue, irregular heartbeats, changes in mental status, and abnormal blood pressure. In severe cases, cardiac arrhythmias or seizures may occur.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











