Fluid and electrolyte balance refers to maintaining the correct volume of fluid and electrolytes cheat and concentration of fluid and electrolytes cheat and in the body, which is vital for physiological functions and overall health.
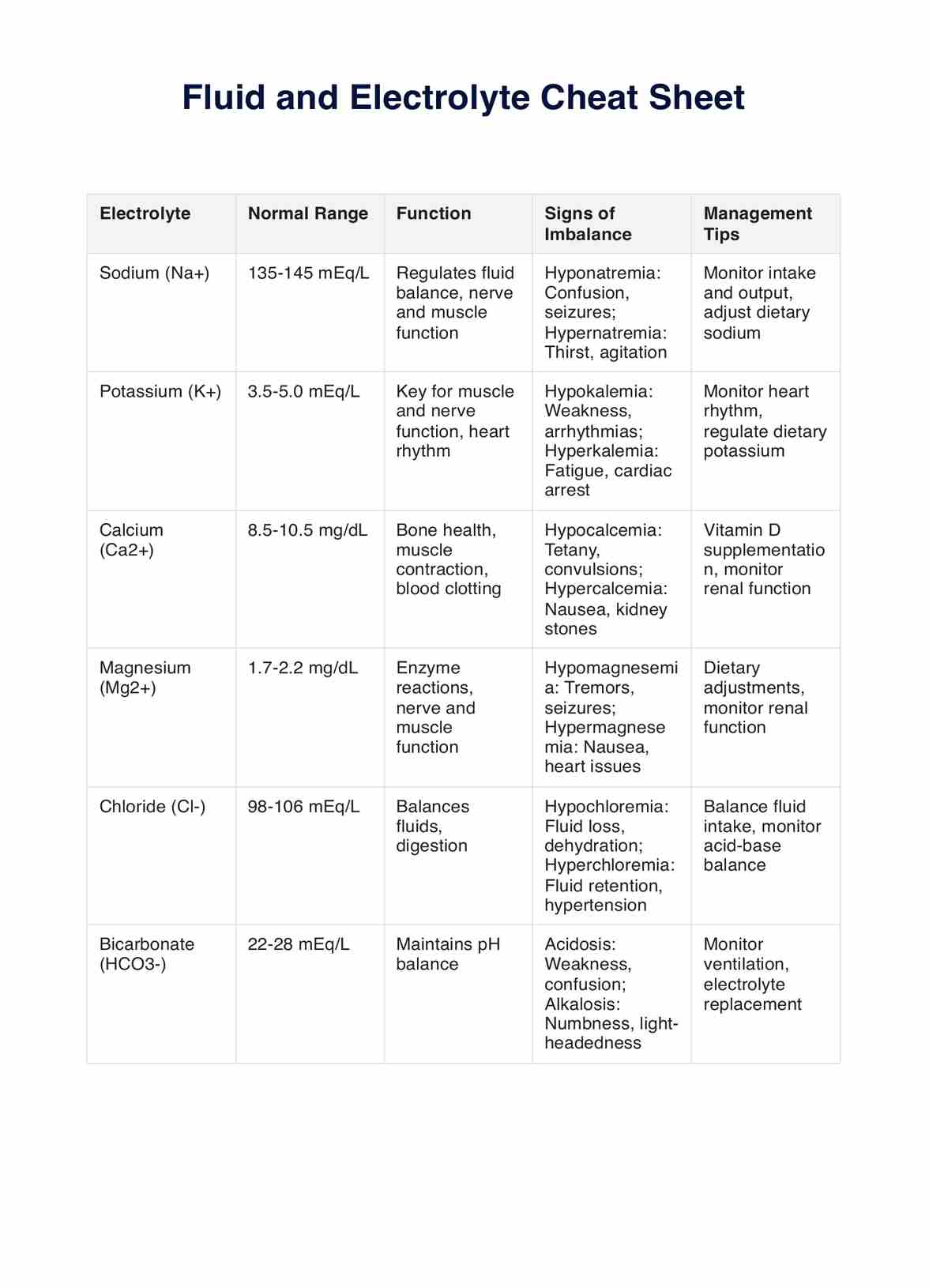
Fluid And Electrolyte Cheat Sheet
Discover Carepatron, the ultimate nursing software with advanced patient portal and telehealth features, streamlining patient care and enhancing efficiency.
Use Template
Fluid And Electrolyte Cheat Sheet Template
Commonly asked questions
Dehydration can lead to various health issues, including urinary and kidney problems, electrolyte imbalances, cognitive impairments, and, in severe cases, hypovolemic shock.
Monitoring fluid intake is crucial in healthcare to prevent dehydration, ensure proper medication efficacy, and maintain electrolyte balance, which is essential for patient health and recovery.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











