When writing progress notes in ABA, it's important to document specific details about the session, including the date, time, duration, goals, and interventions. Progress notes should include objective data on the client's performance, such as the frequency of target behaviors, any changes in behavior, and the effectiveness of the interventions implemented.
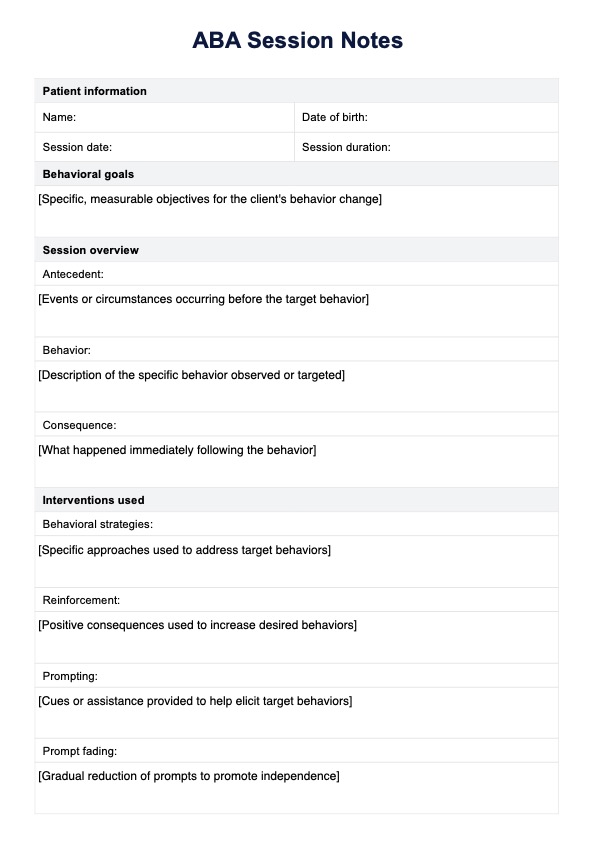
ABA Session Notes
Optimize ABA Session Notes with our comprehensive guide, streamlining documentation for RBTs and BCBAs.
ABA Session Notes Template
Commonly asked questions
An ABA session is typically structured to include several key components: an introduction or review of the previous session, a clear outline of the goals for the current session, and a variety of activities designed to target specific skills or behaviors. The session often begins with a warm-up or rapport-building activity to engage the client. Following this, the clinician implements targeted interventions, such as discrete trial training, natural environment teaching, or behavior modification strategies. The session concludes with a summary of what was accomplished, a review of the client's progress toward goals, and any necessary adjustments for future sessions.
The note should summarize the session's activities, highlighting the specific goals addressed and the strategies used. It should also include objective data on the client's performance, such as the number of trials completed, the percentage of correct responses, and any significant behavioral changes observed. Document the client's engagement level and any challenges faced during the session. Finally, provide recommendations for future sessions, including any modifications to goals or interventions based on the client's progress.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











