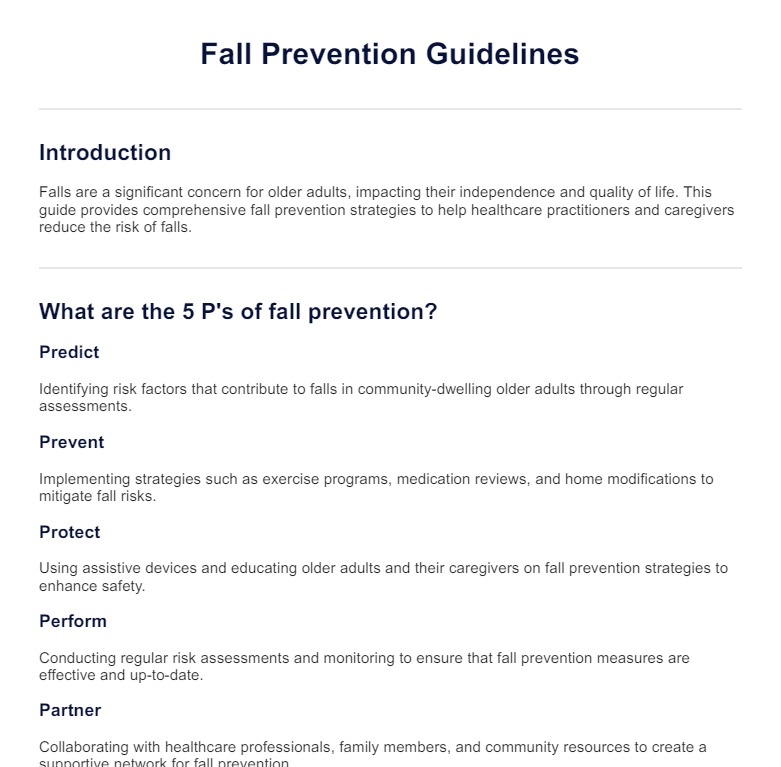
The 5 P's of fall prevention are Predict, Prevent, Protect, Perform, and Partner. These strategies focus on identifying risk factors, implementing preventive measures, ensuring safety, conducting regular assessments, and collaborating with healthcare professionals and caregivers.
Fall Prevention Guidelines PDF
Download Carepatron's free Fall Prevention Guidelines PDF, with examples and tips to help prevent falls. Stay informed and protect yourself and your loved ones.
Fall Prevention Guidelines PDF Template
Commonly asked questions
National guidance for falls prevention typically includes conducting regular risk assessments, implementing multifactorial interventions, and promoting strength and balance exercises. It also emphasizes the importance of medication reviews and home safety modifications.
Common ways to prevent falls include regular exercise to improve strength and balance, home safety modifications like installing grab bars and improving lighting, and managing medications that may cause dizziness or balance issues.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











