The nursing diagnosis for hypoglycemia is "risk for unstable blood glucose" related to factors such as insulin therapy, inadequate food intake, or excessive physical activity.
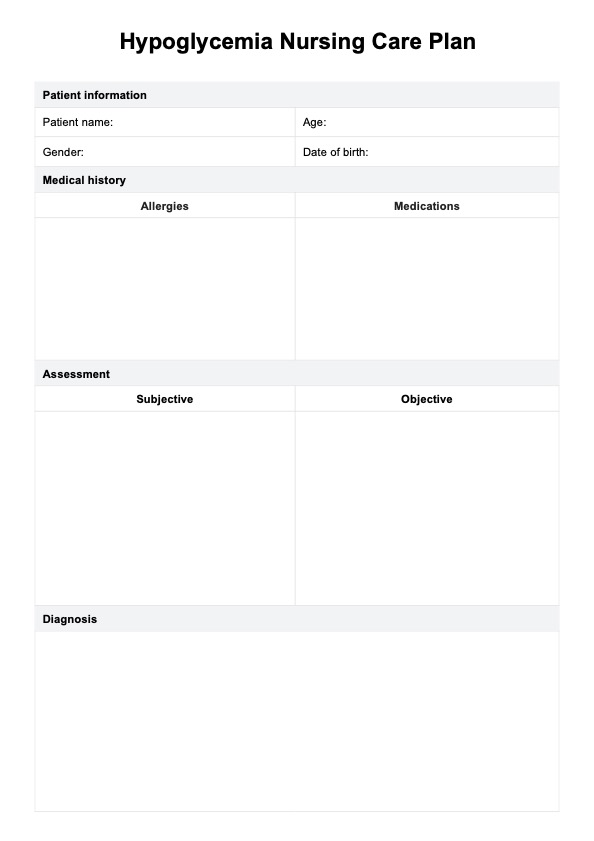
Hypoglycemia Nursing Care Plan
Learn how to manage hypoglycemia effectively with Carepatron's comprehensive nursing care plan. Download a free PDF example today!
Use Template
Hypoglycemia Nursing Care Plan Template
Commonly asked questions
Interventions for hypoglycemia include administering fast-acting carbohydrates like glucose tablets or juice, rechecking blood glucose levels after 15 minutes, and adjusting insulin dosage if necessary.
Oral or intravenous glucose administration is the first-line treatment for hypoglycemia. It raises blood glucose levels and rapidly alleviates symptoms.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments