You must always provide a source if quoting a client, their close relatives, or even a healthcare professional. This professional practice ensures you have a solid foundation for reference if needed in the future.
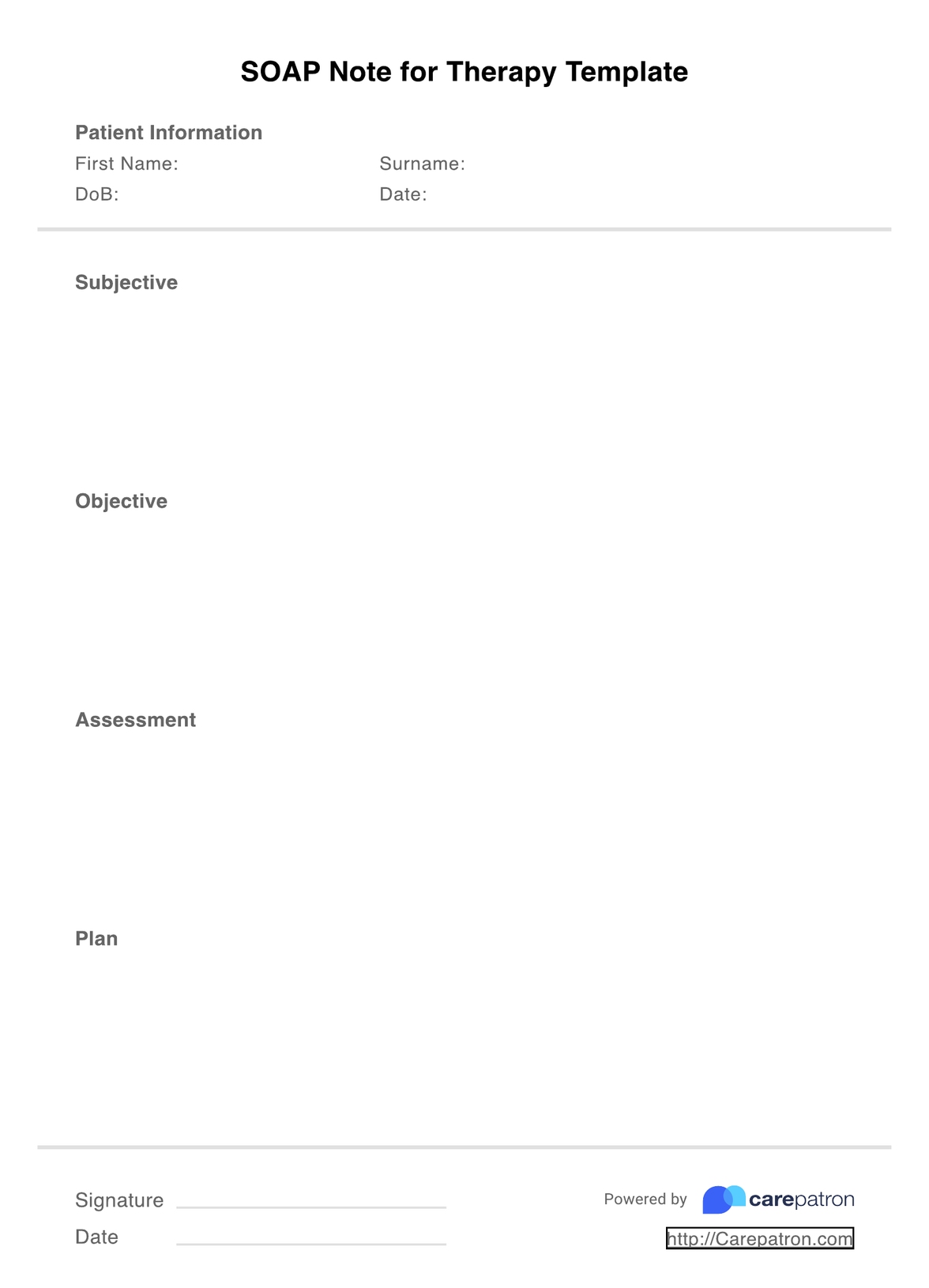
SOAP Notes for Therapy Template
SOAP notes are the best way for therapists to capture clients' mental health. With this template, you can effectively streamline notes and achieve higher clinical outcomes.
SOAP Notes for Therapy Template Template
Commonly asked questions
Some clients may have more clinical information than others, and that's okay. However, a SOAP note should be 1-2 pages, with 3 pages indicating too detailed. Remember that SOAP notes should be an overview, with only necessary information summarized.
While you most certainly can handwrite SOAP notes, electronic is preferred. They are faster to create, and voice-to-text transcription services enable more accurate notes. Carepatron, amongst many other platforms, also provides a clinical documentation storage option, meaning you can protect all information. If you still prefer handwritten, consider scanning and storing these on a secure cloud platform.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











