This is a great question and also an important one. It's important not to waffle in your SOAP notes, so ideally, they should be 1-2 pages long, with 3 pages and beyond becoming excessive.
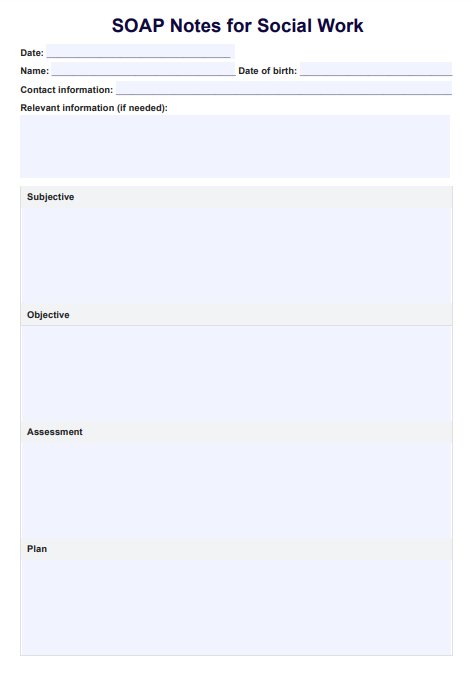
SOAP Notes For Social Work Template
Our SOAP Notes for Social Work Template enhances the quality of your note-taking while streamlining your work.
SOAP Notes For Social Work Template Template
Commonly asked questions
Working within the social work industry may involve working with more than one type of person in a session. However, having one SOAP note for multiple people is not recommended, as this can be a conflict of interest and can result in complications if the individual desires one-on-one treatment later. To keep things simple, stick to one person per SOAP note.
Yes, they absolutely can. It is recommended that they use electronics to reduce time, but this is not a must. If you prefer handwritten documents that are more efficient for you, feel free to do so.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











