This can be quite a difficult question to answer, given it is largely dependent on the type of session you had with your patient. However, it’s important to remember two things: SOAP notes need to cover all important areas of information, and they also need to be concise. Approximately, your SOAP notes should be somewhere between 1-2 pages.
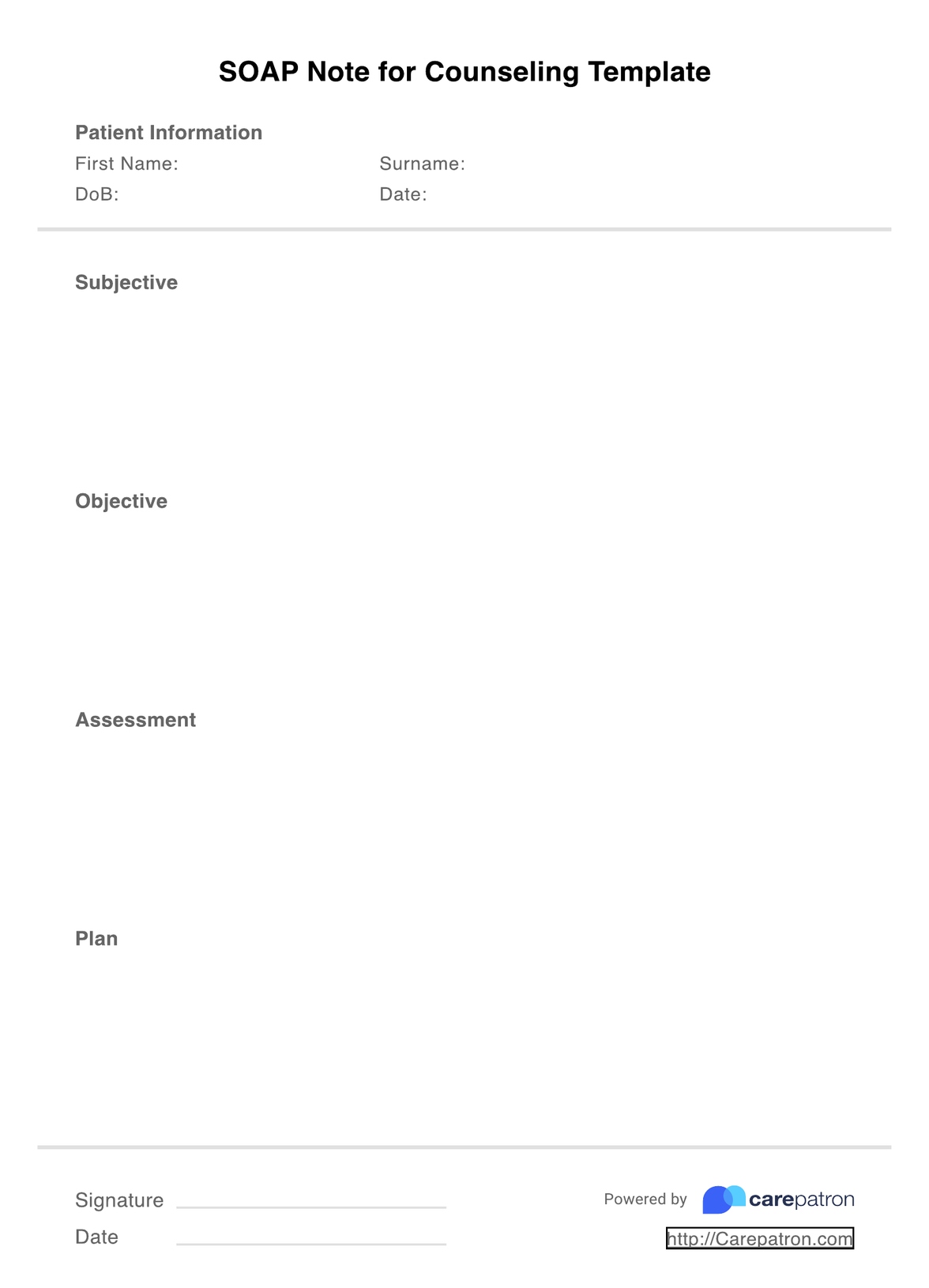
SOAP Notes for Counseling Template
A fantastic PDF SOAP note template for counseling, helping you to simplify documentation and improve clinical outcomes for your patients.
SOAP Notes for Counseling Template Template
Commonly asked questions
The best time to write your SOAP notes is immediately after each session with a patient. This ensures that information is still fresh in your mind and you don’t miss out on any important details. Staying on top of your documentation will also help you stay productive and ensure you don’t have stacks of notes to write at the end of each week.
After you have written your SOAP notes, you need to store them in a HIPAA-compliant manner. In order to keep them protected at all times, we recommend using EHR or practice management software like Carepatron.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











