SOAP is an acronym taught around the world because it is simple enough to remember (however, there is no need to memorize it if you have a nursing SOAP note template with the headings all there for you) and comprehensive enough that if you fill out those four sections thoroughly with key information, you'll have great clinical notes.
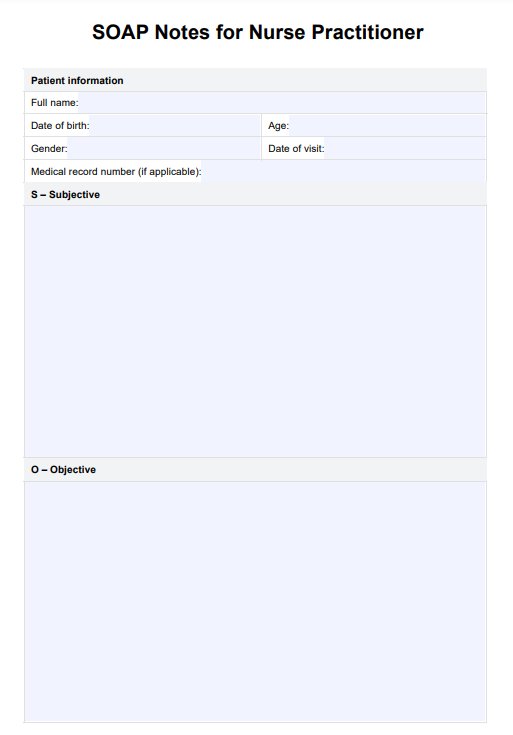
SOAP Notes for Nurse Practitioner Template
Download a SOAP Notes for Nursing Template to streamline nursing documentation. Ensure clear and organized records for quality patient care.
SOAP Notes for Nurse Practitioner Template Template
Commonly asked questions
The four parts of SOAP are subjective, objective, assessment, and plan. These sections help organize patient information and clinical findings for clear communication.
To write a good assessment SOAP note, clearly summarize your clinical findings and thoughts about the patient's condition, linking the subjective and objective information. Use concise language and focus on key points to make your assessment clear and effective. You can find many examples of SOAP notes for nurse practitioner online.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











