A psychotherapy note is a detailed record of a patient's psychotherapy session, including the patient's symptoms, treatment goals, and progress. It should include the date and time of the session, the patient's attendance and participation, and any notable events or behaviors. The note should also document the therapist's observations, impressions, and any relevant psychological or medical information.
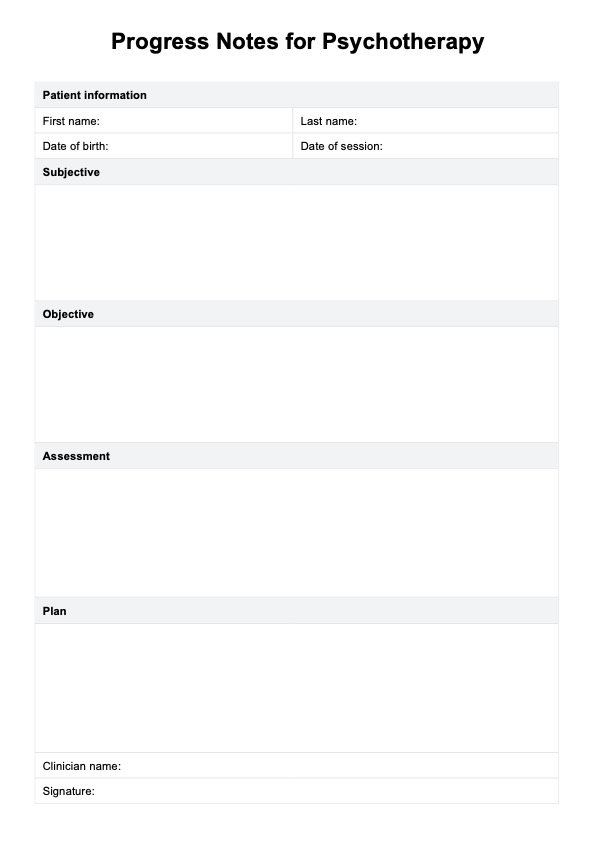
Progress Notes For Psychotherapy Template
Our psychotherapy progress note template will streamline your workflow, create efficient notes faster, and enhance the quality of your care without compromise.
Progress Notes For Psychotherapy Template Template
Commonly asked questions
A psychotherapy note is a detailed record of a patient's psychotherapy session, while a progress note summarizes the patient's overall progress and treatment plan. Psychotherapy notes are typically more detailed and focused on the specific session, while an individual progress note provides a broader overview of the patient's treatment and progress. Unlike progress notes, psychotherapy notes are kept confidential and not shared with other healthcare providers.
To write effective counseling notes, identify the key issues and goals discussed during the session. Use a clear and concise writing style, and include specific details about the patient's symptoms, behaviors, and progress. You can also use a counseling case notes template or a counselor notes template as a guide. Document any notable events or behaviors, and include any relevant psychological or medical information. Finally, review and edit your notes to ensure accuracy and completeness and keep them confidential and secure.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











