Other tools for assessing dissociation include the Dissociative Experiences Scale (DES), the Structured Clinical Interview for DSM-Dissociative Disorders (SCID-D), and the Clinician-Administered Dissociative States Scale (CADSS).
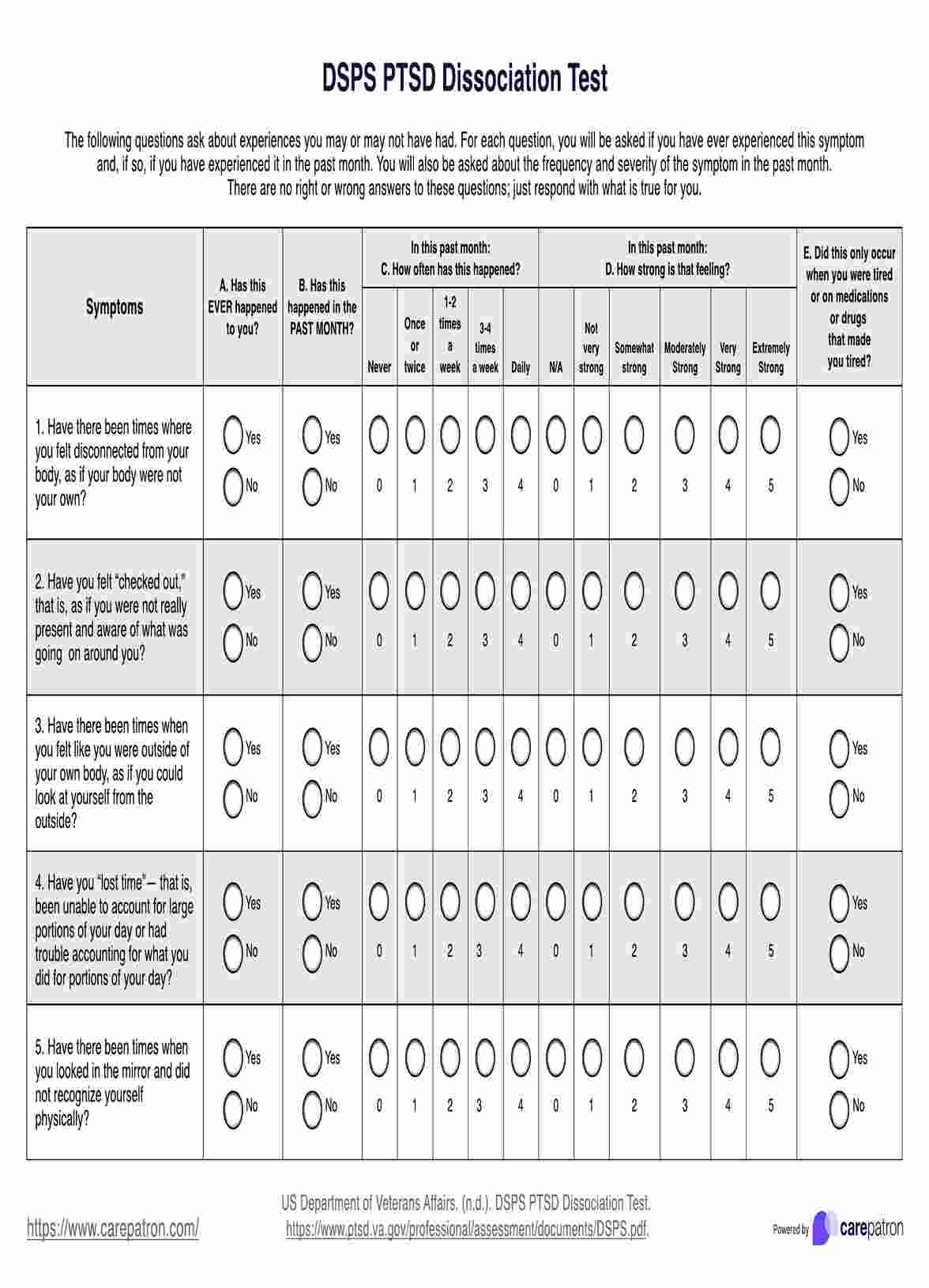
PTSD Dissociation Test
Assess PTSD dissociation symptoms with Carepatron's free PDF download containing a test and examples for evaluation. Get insights and guidance on recognizing symptoms.
Use Template
PTSD Dissociation Test Template
Commonly asked questions
The four dissociation stages are amnesia, depersonalization, derealization, and identity confusion.
You may be dissociating if you feel disconnected from your thoughts, emotions, or surroundings, experience memory lapses, or feel as though you are observing yourself from outside your body.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











