No. Trauma is the most common trigger, but it’s not always the cause of it. Being fatigued or dealing with specific stressors can cause dissociation.
Dissociation Worksheet PDF
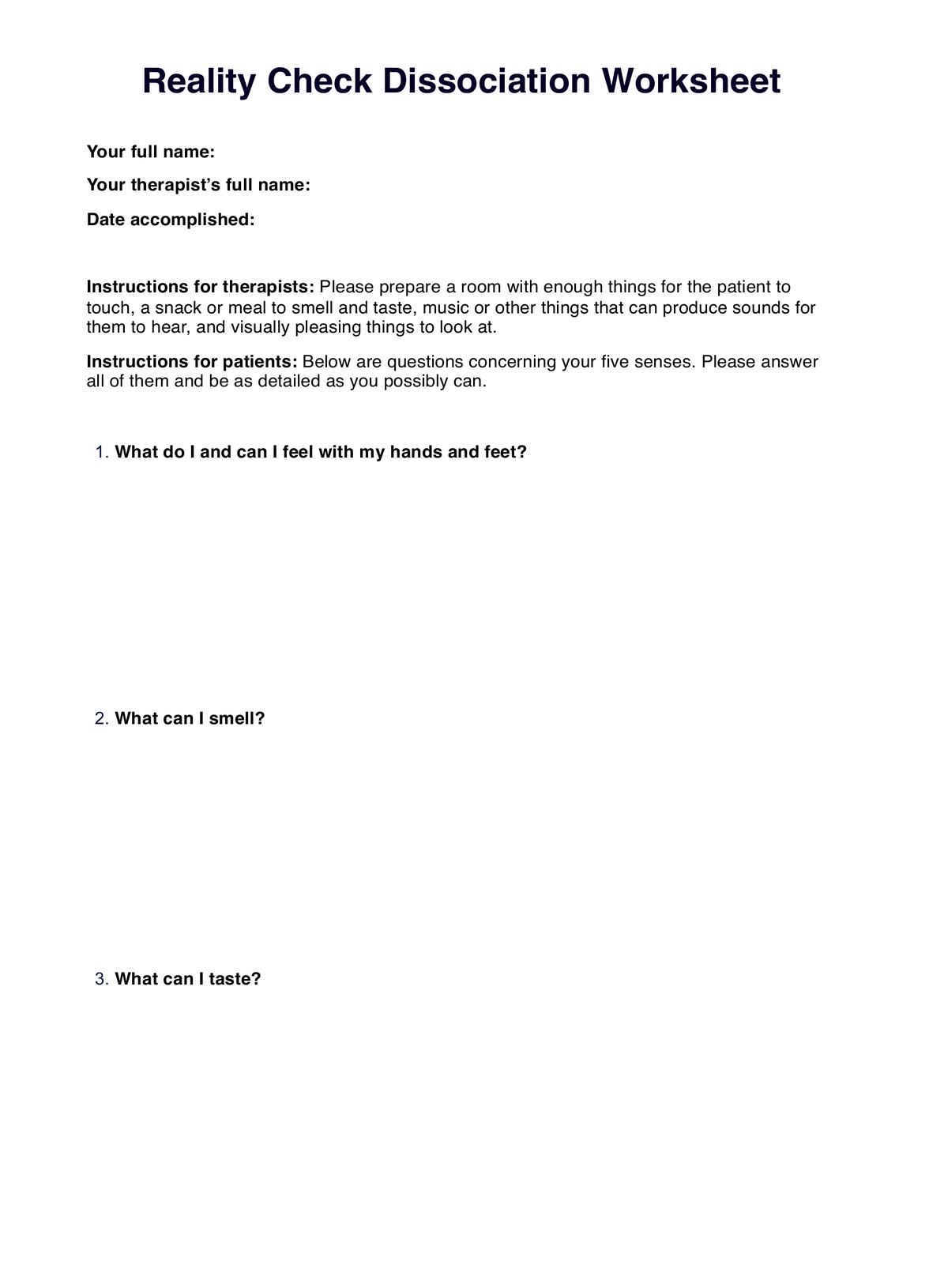
Learn about dissociation and use this Dissociation Worksheet to help yourself or your patients snap out of a dissociated state.
Use Template
Dissociation Worksheet PDF Template
Commonly asked questions
Yes. These can contribute to dissociative experiences, but they are temporary and resolve on their own when the effects wear off.
That depends on the severity. Dissociation can disrupt a person’s day and prevent them from doing what they must do. Extreme cases can result in risky and destructive behavior like self-harm, reckless driving, not looking both ways while crossing the street, and substance abuse.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











