The most effective treatment for DMDD often involves a combination of cognitive behavioral therapy and, if necessary, stimulant medications. Tailored to individual needs, these approaches aim to reduce symptoms, improve emotional regulation, and enhance overall functioning.
DMDD Treatment Plan
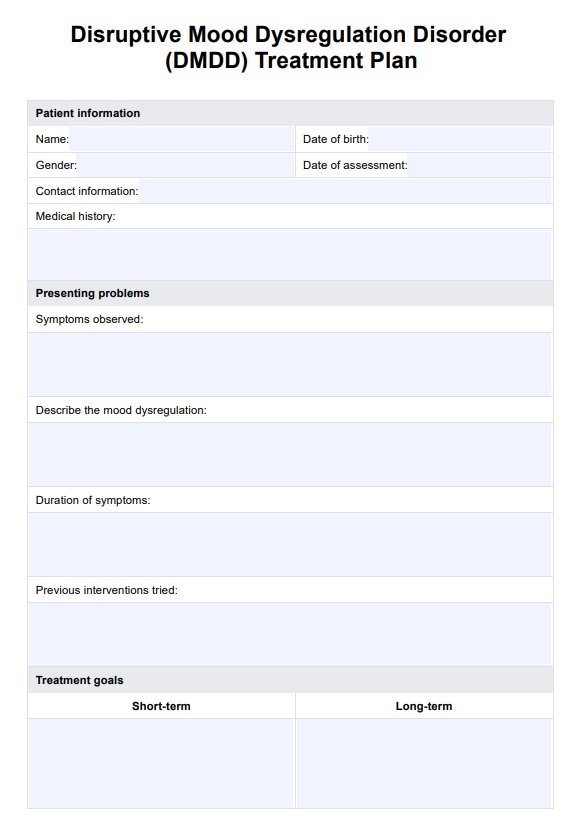
Create an effective treatment plan for patients with disruptive mood dysregulation disorder (DMDD). Get Carepatron's PDF template for free!
DMDD Treatment Plan Template
Commonly asked questions
No, DMDD is not the same as bipolar disorder; they are distinct conditions. DMDD is characterized by chronic irritability and frequent, severe temper outbursts, while bipolar disorder involves episodic mood changes that include emotional highs (mania) and lows (depression).
While trauma is not specifically identified as a cause of DMDD, stressful life events, and environmental factors can exacerbate or trigger the onset of symptoms in vulnerable children and adolescents.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











