Therapists, counselors, and mental health professionals utilize this tool to enhance the efficiency and accuracy of their clinical documentation.
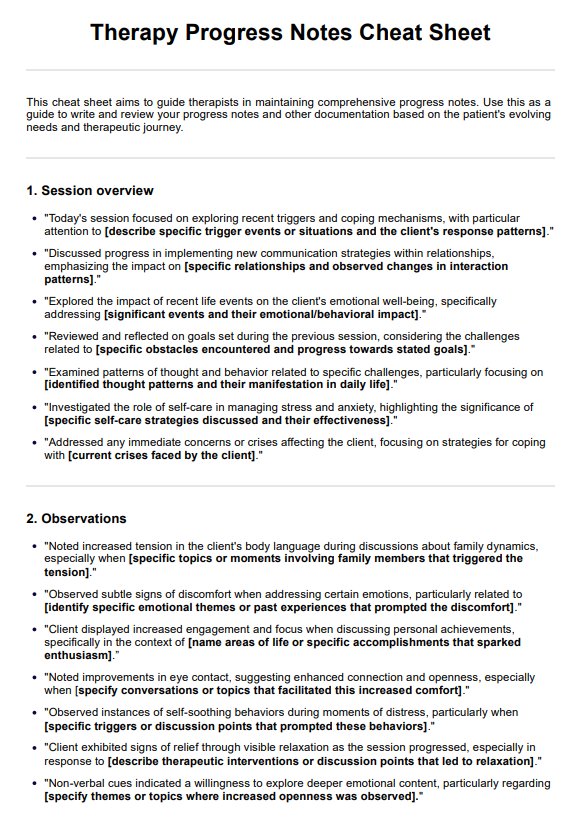
Therapy Progress Notes Cheat Sheet
Streamline your documentation process with our Therapy Progress Notes Cheat Sheet! Download a free PDF copy here.
Use Template
Therapy Progress Notes Cheat Sheet Template
Commonly asked questions
Use it during and after client sessions to ensure comprehensive, structured progress note documentation.
It streamlines the documentation process, offering prompts and a user-friendly structure, ultimately improving the quality and consistency of clinical documentation.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











