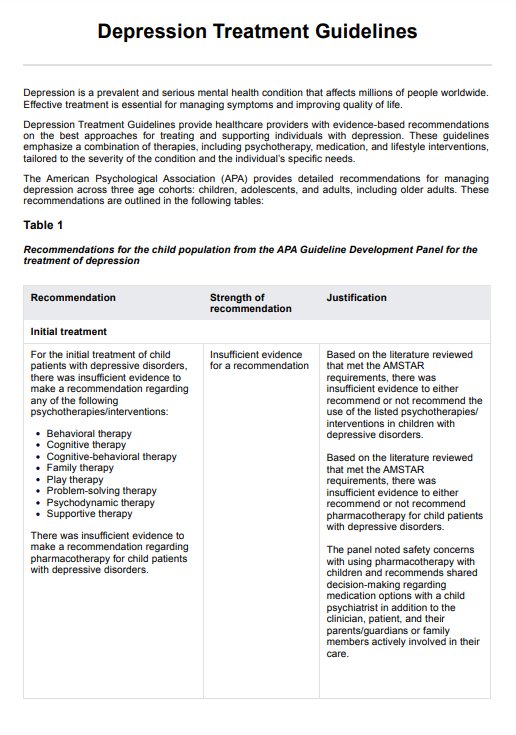
Depression treatment guidelines provide evidence-based recommendations for healthcare professionals on how to effectively treat major depressive disorder using a combination of pharmacological treatments, psychological treatments, and adjunctive treatments.
Depression Treatment Guidelines
Learn about Depression Treatment Guidelines for effective management and treatment of depressive disorders. Download a free handout here.
Depression Treatment Guidelines Template
Commonly asked questions
The most common depression therapies include cognitive behavioral therapy (CBT), selective serotonin reuptake inhibitors (SSRIs), mindfulness-based cognitive therapy (MBCT), and electroconvulsive therapy (ECT) for severe or treatment-resistant cases.
Treatment for depression is adjusted based on the intensity of the symptoms, the patient's preferences, and the treatment response. Options range from psychotherapy and antidepressant medication to more advanced treatments such as repeated transcranial magnetic stimulation. This approach is essential for managing mental disorders, ensuring that the treatment plan aligns with the specific needs of the patient.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











