The standard treatment for dementia involves a combination of pharmacological and non-pharmacological interventions aimed at managing symptoms and improving quality of life. This may include medications to address cognitive decline and behavioral symptoms and therapies such as cognitive stimulation and occupational therapy.
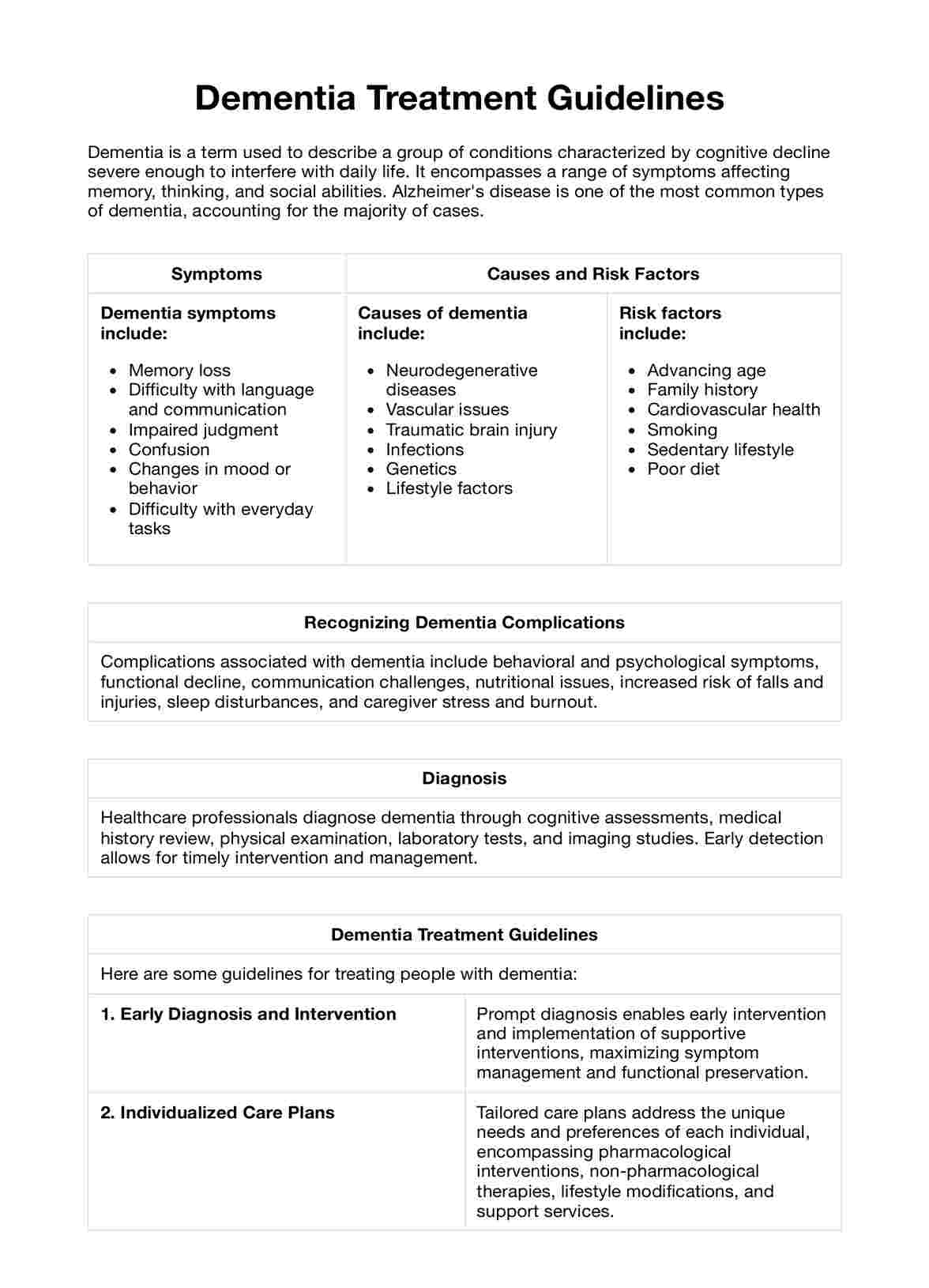
Dementia Treatment Guidelines
Explore comprehensive dementia treatment guidelines and use Carepatron's free PDF download of an example plan. Learn about effective strategies and interventions for dementia care.
Dementia Treatment Guidelines Template
Commonly asked questions
While there is no definitive cure for dementia, cholinesterase inhibitors (e.g., donepezil, rivastigmine) and N-methyl-D-aspartate (NMDA) receptor antagonists (e.g., memantine) are considered the gold standard of pharmacological treatment for Alzheimer's disease, the most common form of dementia. These medications may help improve cognitive function and alleviate symptoms in some individuals.
In the early stages of dementia, non-pharmacological interventions such as cognitive stimulation, physical exercise, and social engagement are often recommended as the first line of treatment. These interventions can help maintain cognitive function, promote independence, and enhance overall well-being.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











