Cognitive-behavioral therapy and interpersonal therapy are among the most effective treatment approaches for PDD, often in conjunction with medication.
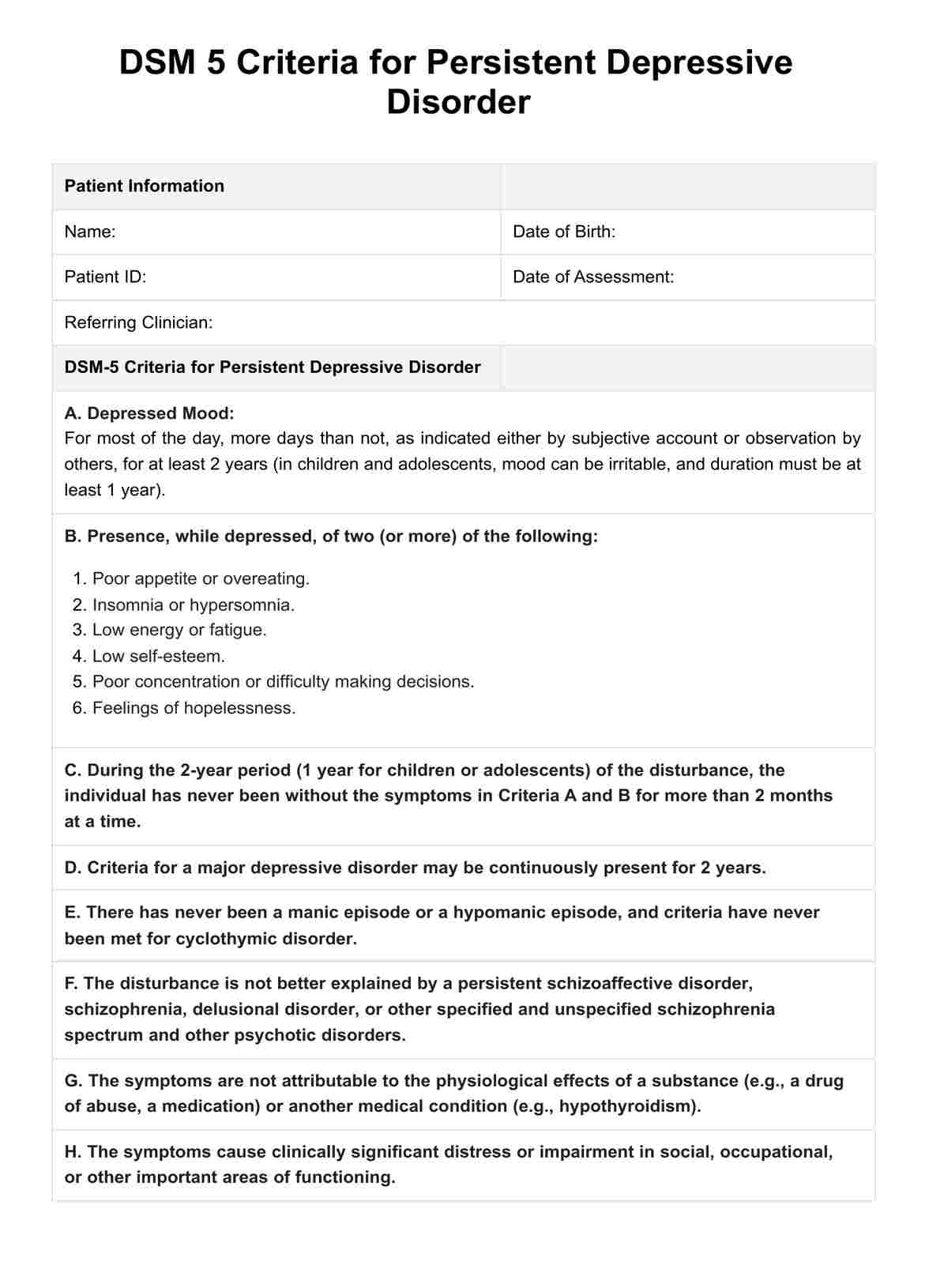
DSM 5 Criteria for Persistent Depressive Disorder
Explore the symptoms, diagnosis, and treatment of Persistent Depressive Disorder (PDD) with our comprehensive guide and free PDF download.
Use Template
DSM 5 Criteria for Persistent Depressive Disorder Template
Commonly asked questions
Regular aerobic exercises, such as walking, running, or swimming, have been shown to help reduce depressive symptoms and improve mood.
You can be diagnosed when depressive symptoms persist for most of the day, more days than not, for at least two years in adults and one year in children and adolescents, alongside other DSM-5 criteria.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











