Binge eating refers to consuming large amounts of food in a short period while feeling a lack of control over eating. Feelings of distress, guilt, or shame often accompany it.
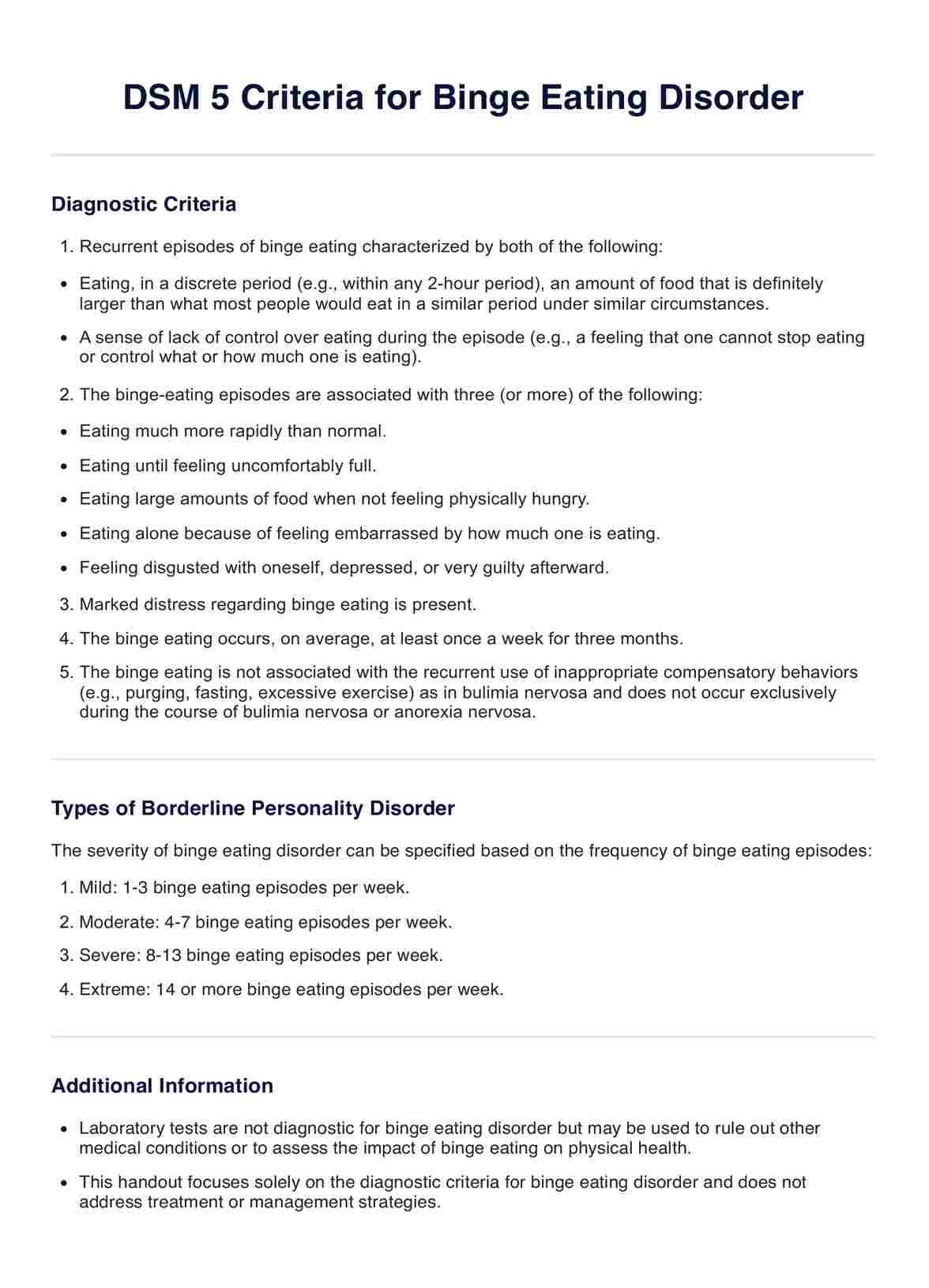
DSM 5 Criteria for Binge Eating Disorder
Explore the DSM-5 Criteria for Binge Eating Disorder with our comprehensive template. Understand the diagnosis, impact, and treatment options for BED.
DSM 5 Criteria for Binge Eating Disorder Template
Commonly asked questions
The DSM-5 recognizes three distinct eating disorders: Anorexia Nervosa, Bulimia Nervosa, and binge eating disorder. Each disorder has specific diagnostic criteria and patterns of disordered eating behaviors.
Yes, other specified feeding or eating disorder (OSFED) is in DSM-5. It encompasses eating disorders that do not meet the full criteria for Anorexia Nervosa, Bulimia Nervosa, or binge eating disorder but still cause significant distress or impairment.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











