BPD is unique due to its intense emotional reactions, fear of abandonment, and unstable relationships.
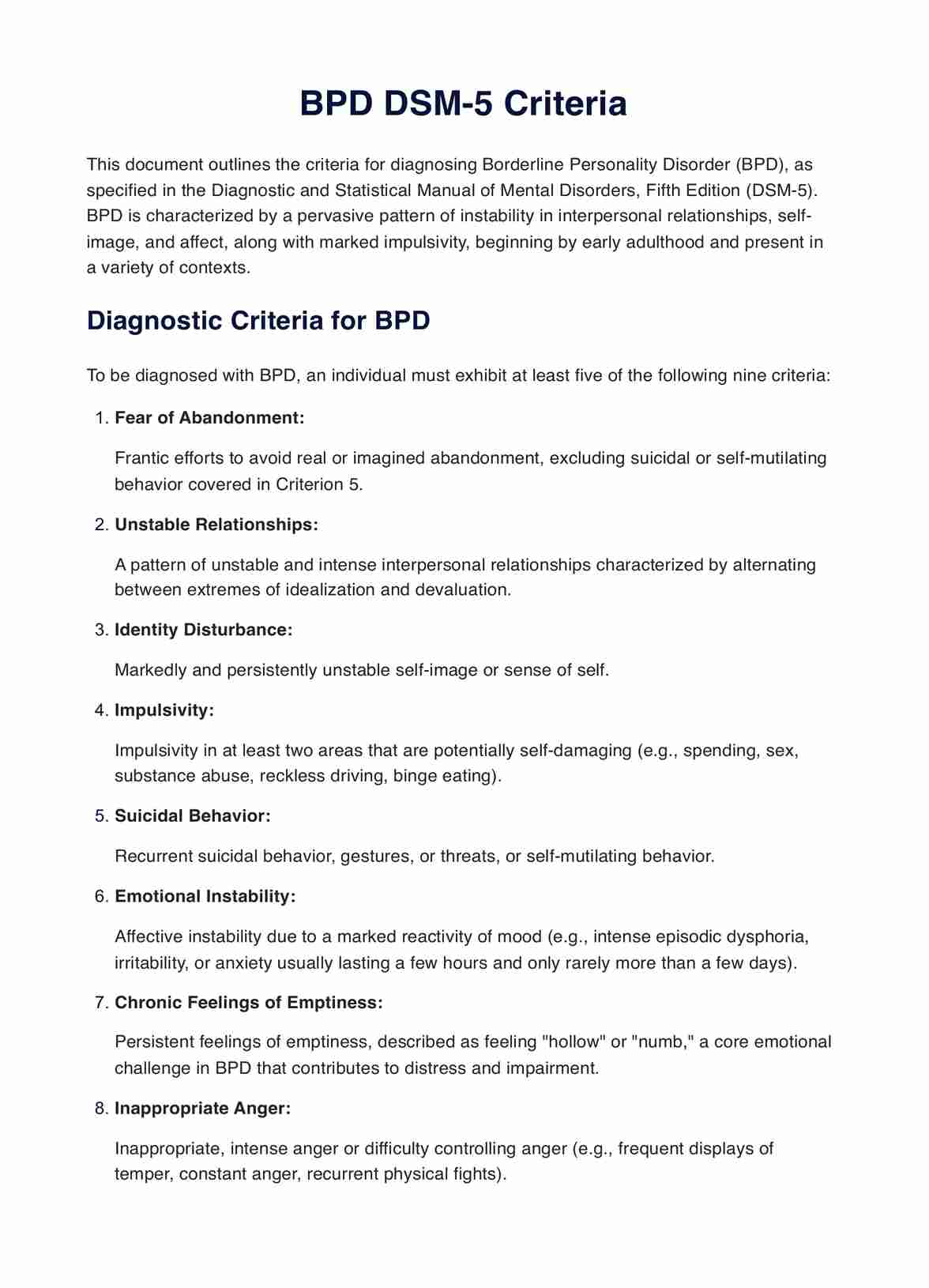
BPD DSM-5 Criteria PDF
Simplify mental health practice management with Carepatron. Secure, easy-to-use software for telehealth, documentation, and collaboration.
Use Template
BPD DSM-5 Criteria PDF Template
Commonly asked questions
Yes, with a combination of psychotherapy, medication, and support, many individuals with BPD can lead fulfilling lives.
Not necessarily. Many people see significant improvement in their symptoms and quality of life with appropriate treatment.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











