PGD is typically triggered by the death of a loved one. Risk factors for developing prolonged grief disorder include personal vulnerability, the nature of the death, and a person's coping skills, which may influence whether they develop PGD.
Prolonged Grief Disorder DSM 5 Criteria
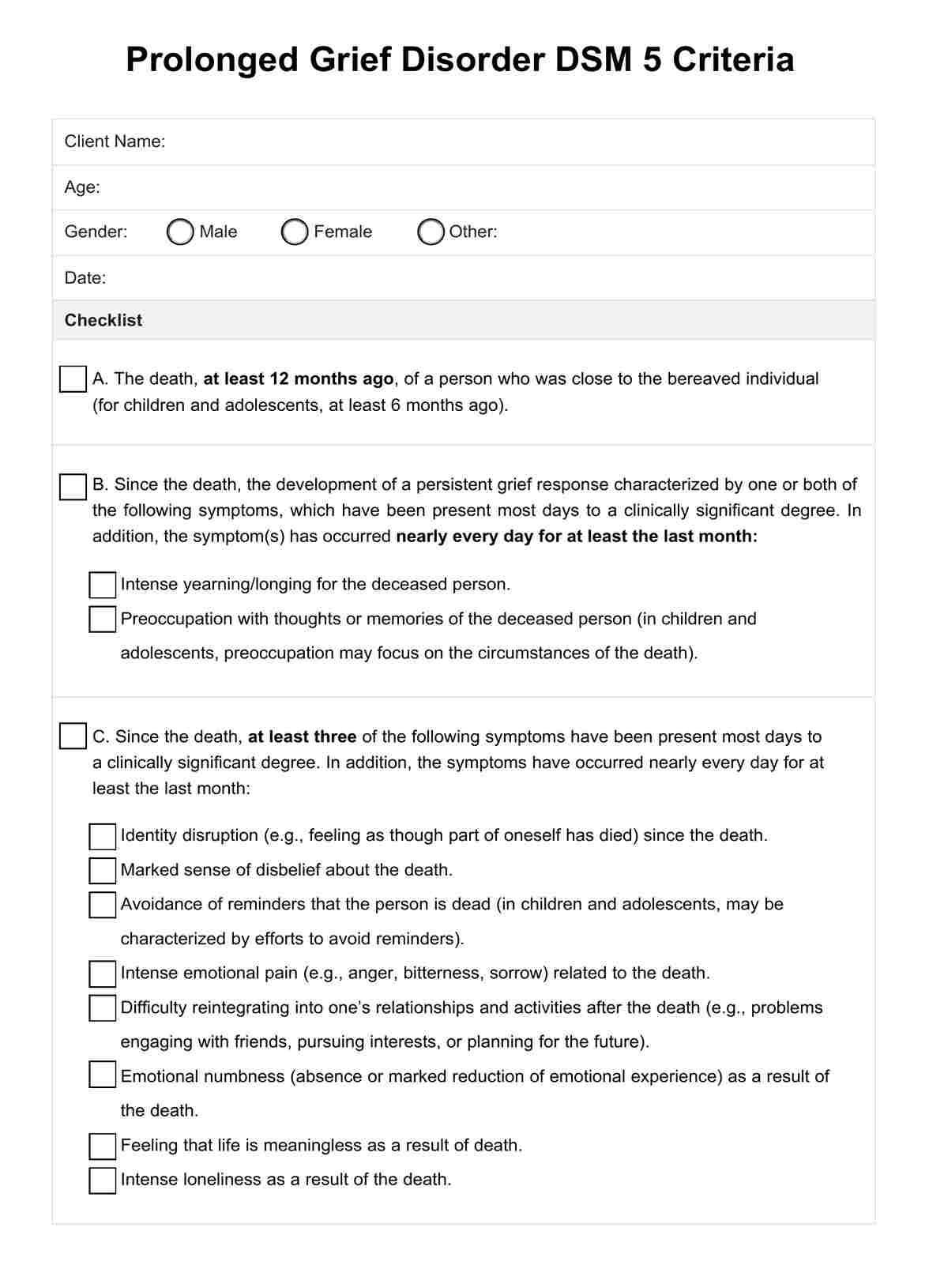
Access a helpful checklist tool to help in diagnosing prolonged grief disorder among clients. Download your free PDF here.
Prolonged Grief Disorder DSM 5 Criteria Template
Commonly asked questions
Grief can differ drastically between individuals, but it is generally expected to lessen across the first year following the death. If symptoms persist at a clinically significant level for at least 12 months in adults and six months in children and adolescents, it may be classified as PGD.
Yes, there are effective treatments for PGD. Prolonged and complicated grief treatment may include psychotherapy approaches (like cognitive-behavioral therapy or complicated grief therapy), medication (antidepressants), support groups, and self-care strategies such as mindfulness.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











