Look for patterns of behavior that hinder their progress or happiness, accompanied by negative self-talk or withdrawal from enjoyed activities.
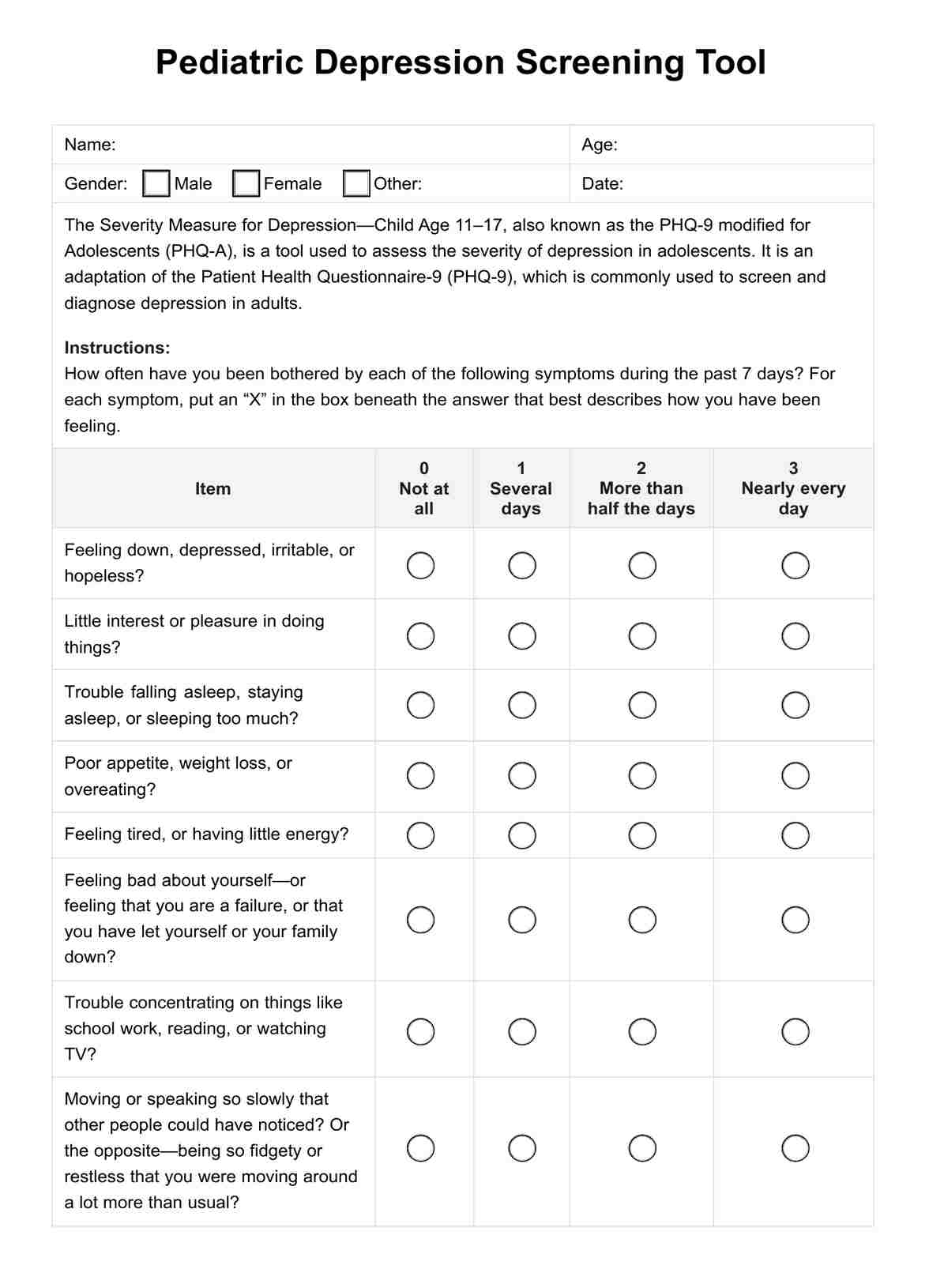
Pediatric Depression Screening Tool
Explore the benefits of Pediatric Depression Screening Tools for early detection and effective treatment in children and adolescents.
Use Template
Pediatric Depression Screening Tool Template
Commonly asked questions
It often stems from genetic predispositions, environmental factors, and psychological stressors.
Underlying mental health issues, negative self-perception, and unaddressed emotional trauma can lead to self-sabotage.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











