While there's no cure, effective management is possible with the right treatment plan.
Bipolar Treatment Guidelines
Explore expert Bipolar Treatment Guidelines, including diagnosis, symptom management, and personalized care strategies for improved health.
Use Template
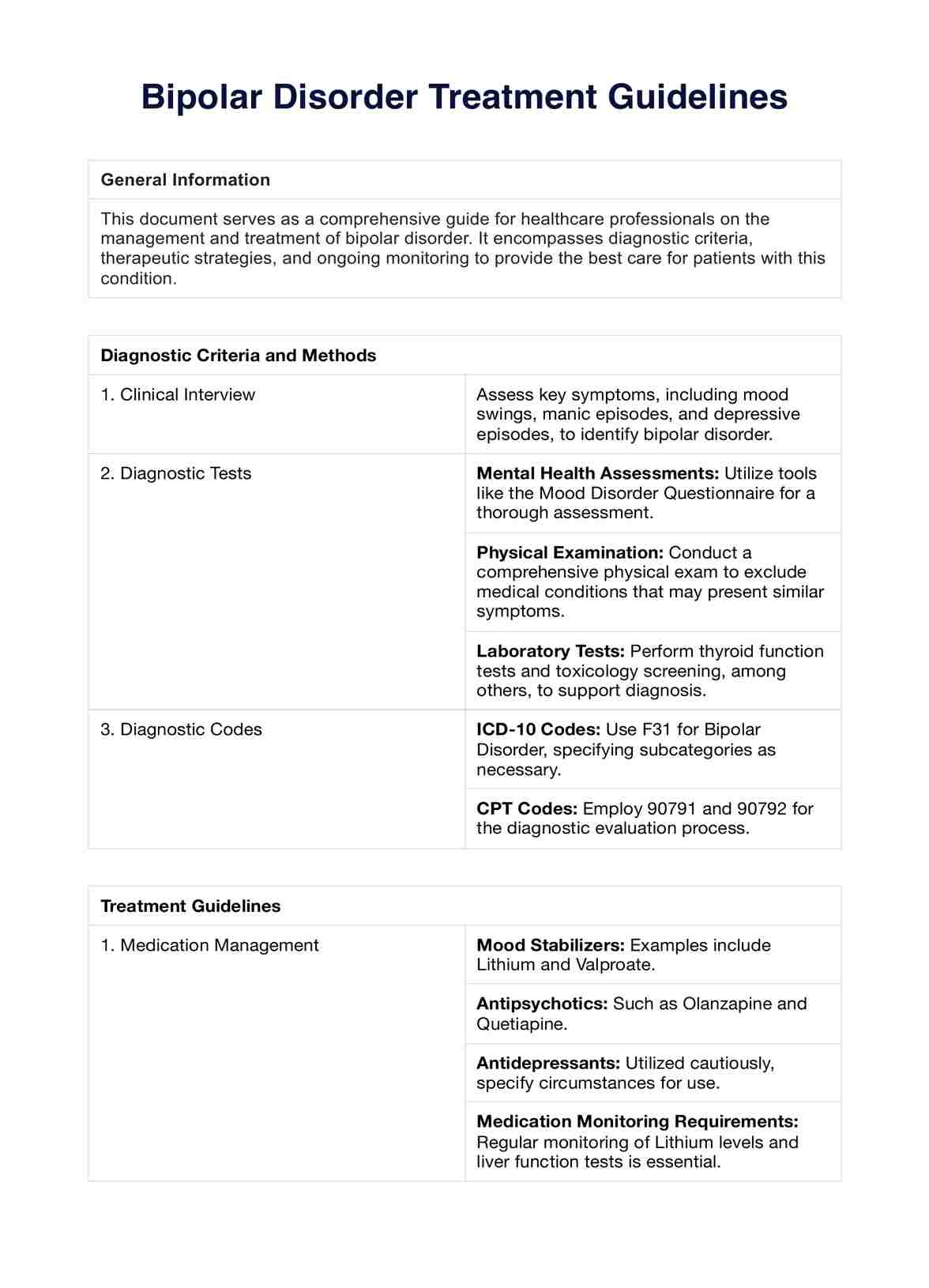
Bipolar Treatment Guidelines Template
Commonly asked questions
Treatment is often lifelong to manage symptoms and prevent relapse.
Yes, healthy lifestyle choices complement medical treatments and can help stabilize mood swings.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











