The causes of mood disorders are believed to be a combination of genetic, biological, environmental, and psychological factors. This can include a family history of mood disorders, brain chemistry imbalances, stressful life events, and chronic health conditions.
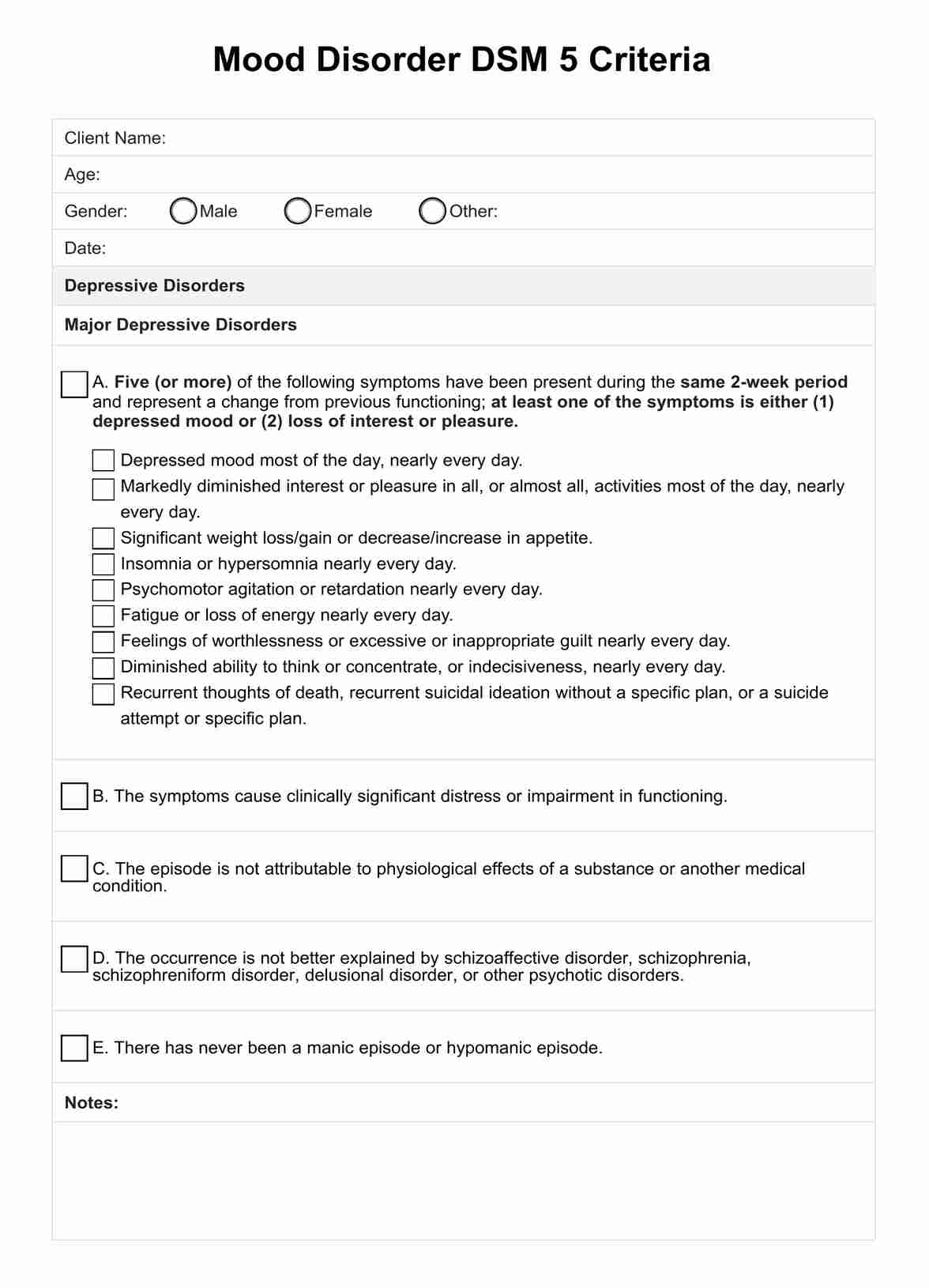
Mood Disorder DSM 5 Criteria
Explore a comprehensive reference tool to help diagnose bipolar and depressive disorders.
Mood Disorder DSM 5 Criteria Template
Commonly asked questions
While some mood disorders can be managed more effectively than others, most can be substantially improved with proper treatment. This might include medication, psychotherapy, or a combination of both, allowing many individuals to lead normal, productive lives.
Yes, lifestyle changes such as regular physical activity, maintaining a healthy diet, getting enough sleep, and reducing stress can positively impact managing mood disorders. However, lifestyle changes should complement, not replace, professional treatment plans.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











