PMS involves mild to severe mood disorder with moderate symptoms like bloating and mood swings, while PMDD is a severe form with intense mood disturbances like irritability and depression.
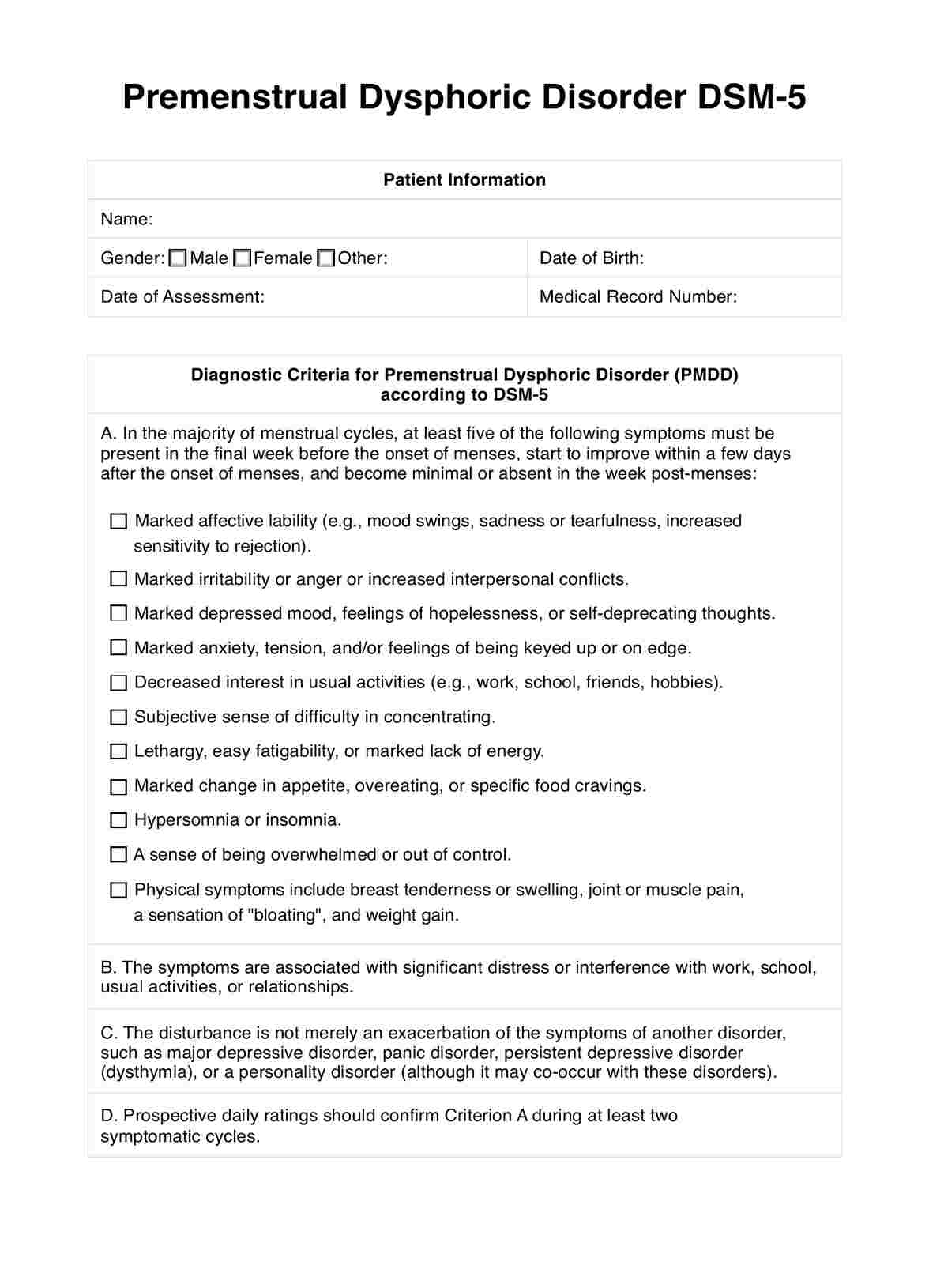
Premenstrual Dysphoric Disorder DSM-5
Explore the criteria of Premenstrual Dysphoric Disorder (PMDD) as outlined in DSM-5, shedding light on panic disorder and its impact on mental health.
Use Template
Premenstrual Dysphoric Disorder DSM-5 Template
Commonly asked questions
PMDD is differentiated by its specific symptoms occurring in the late luteal phase and resolving shortly after menstruation, distinct from other mood disorders or menstrual conditions.
Yes, PMDD is classified as a mental illness in the DSM-5 due to its significant impact on mood and functioning during the menstrual cycle.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











