Hoarding is often linked to OCD, characterized by persistent difficulty discarding possessions, regardless of their actual value. It is also considered a feature of obsessive-compulsive personality disorder (OCPD). It can develop alongside other mental conditions, like dementia and schizophrenia.
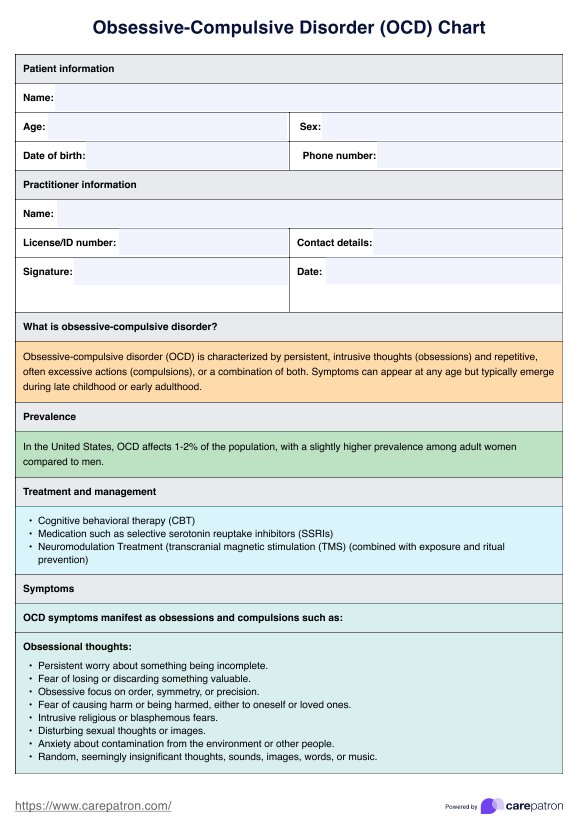
OCD Chart
Incorporate our OCD Chart into your practice as an essential reference and documentation tool to support client progress. Download your free chart today!
Use Template
OCD Chart Template
Commonly asked questions
OCD often co-occurs with other mental health conditions like generalized anxiety disorder, body dysmorphic disorder, and hoarding disorder, complicating diagnosis and treatment.
Cognitive behavioral therapy (CBT) is one of the widely used treatments for OCD. It helps individuals identify and challenge the irrational thoughts and behaviors contributing to their compulsions.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











