What is obsessive compulsive disorder (OCD)?
Obsessive-compulsive disorder (OCD) is a mental disorder that impacts millions globally. OCD is defined by patterns of uncontrollable, recurrent thoughts (obsessions) and behaviors (compulsions) that the individual feels the urge to repeat over and over. These obsessions and compulsions are time-consuming and often significantly disrupt the individual’s daily activities and social interactions.
The experience is far from the occasional worry or ritualistic behavior that people without the disorder experience. For someone with OCD, ordinary objects and common situations can become triggers for their obsessions. These obsessions are not simply concerns or worries about real-life problems but are often exaggerated fears. For instance, they could believe that being unable to perform a task in a very specific manner could harm themselves or others around them.
The compulsions, which are repetitive behaviors or mental acts, are efforts to counteract or offset the anxiety provoked by these obsessions. For example, individuals might repeatedly wash their hands, check locks, or perform mental rituals like counting or praying in a specific pattern. While these actions might provide temporary relief, this is short-lived, which leads to a reinforcing cycle where the compulsive behaviors become more ingrained.
What is the difference between obsessions and compulsions?
When discussing obsessive-compulsive disorder (OCD), we often encounter two essential concepts: obsessions and compulsions.
Obsessions are essentially intrusive and unwanted thoughts, images, or urges that repeatedly appear in the mind. People with OCD usually find these obsessions disturbing, and they often manifest as fears of contamination, worries about safety, or disturbing religious or sexual thoughts. Unlike the everyday worries that we all experience, these intrusive thoughts are persistent and can cause significant anxiety and distress.
Imagine a patient who can't shake the idea that they've left the stove on despite having checked multiple times. This thought is more than a momentary concern. It is an obsession that can constantly be on their minds and cause distress.
Compulsions, on the other hand, are behaviors or mental acts that individuals feel compelled to perform in response to their obsessions or according to strict rules. These actions are done in an effort to reduce distress or prevent a feared event or situation from happening. Compulsions might provide brief relief from the anxiety but they are often not rationally connected to the problem they are meant to address.
Take the example of someone compelled to wash their hands exactly seven times to feel clean enough to be safe from contamination. This ritualistic behavior is a compulsion—a response to the obsession with contamination.
Symptoms of OCD
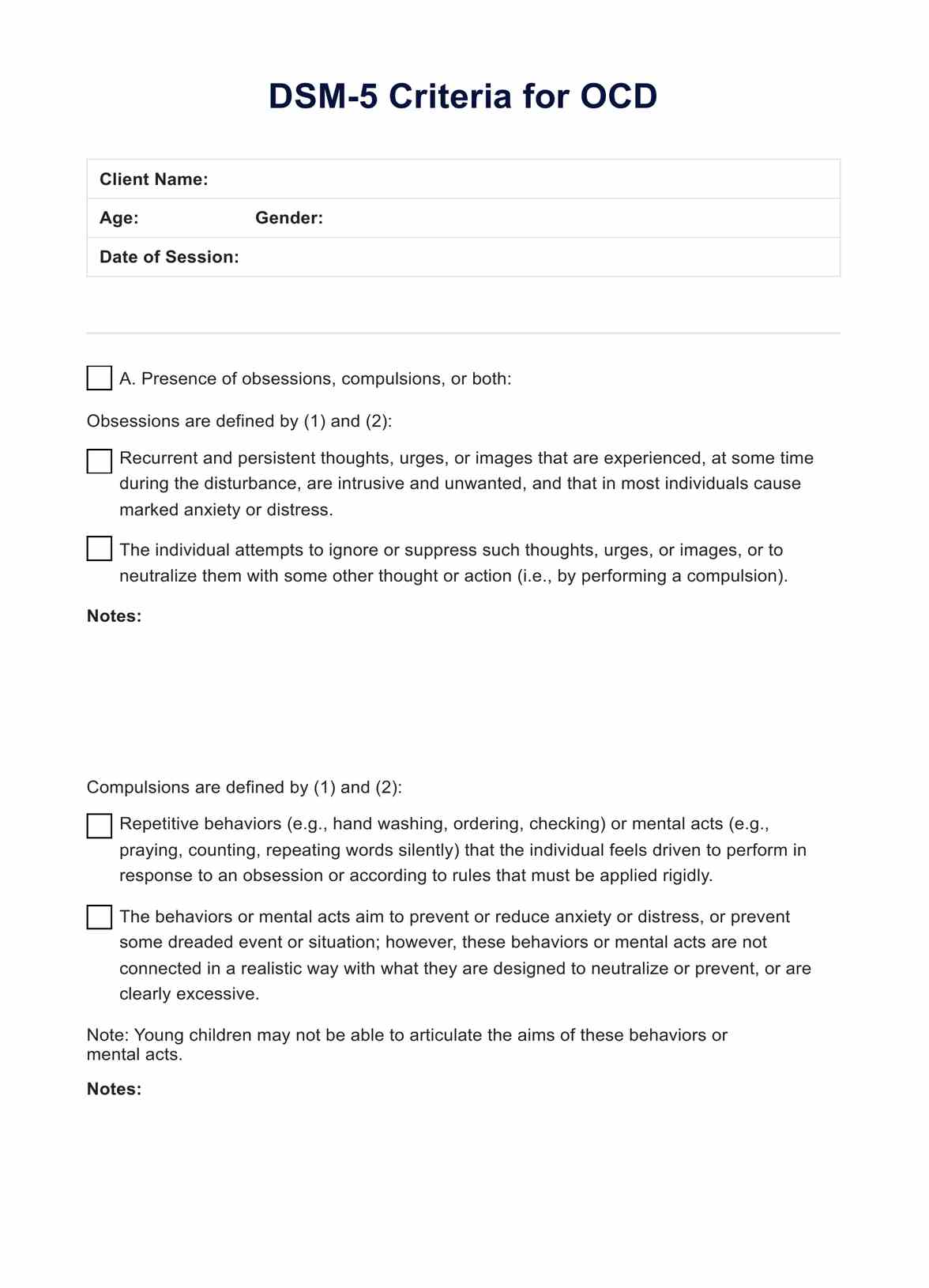
The Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (DSM-5), is the authoritative manual of mental disorders by the American Psychiatric Association (2013), which is now widely used by healthcare professionals. The DSM-5 then provides us with a well-defined set of criteria characterizing the symptoms to diagnose OCD.
The DSM-5 highlights the presence of obsessions and compulsions along with significant distress and impairment. To begin with, obsessions should be characterized by the following:
- Persistent, intrusive thoughts, impulses, or images: This means these are unwanted ideas or visions that keep coming up in the mind of the person with OCD.
- Attempts to ignore or suppress: The person might try to suppress these unwelcome thoughts or counteract them with other thoughts or actions, leading to compulsive behavior.
On the other hand, compulsions are classified as:
- Repetitive behaviors or mental acts: These are repeated actions (like handwashing or checking locks) or mental rituals (like counting or repeating words) that someone needs to perform in response to the obsession.
- Aimed at preventing or reducing distress: More importantly, these actions are carried out to soothe the distress caused by obsessions or to prevent a feared event from happening.
Further diagnostic considerations specifically for OCD include the following:
- Time consumption: The obsessions or compulsions take up more than one hour per day or cause clinically significant distress or impairment in social, occupational, or other important areas of functioning.
- Not attributable to other factors: The disturbance is not attributable to the physiological effects of a substance (e.g., drug abuse, medication) or another medical condition.
- Differentiation from other disorders: The symptoms cannot be better explained by the symptoms of another mental disorder (e.g., generalized anxiety disorder, body dysmorphic disorder).
What is the difference between OCD and obsessive-compulsive personality disorder?
It's crucial to differentiate between obsessive-compulsive disorder (OCD) and obsessive-compulsive personality disorder (OCPD). Despite their similar names, they are distinct disorders with unique diagnostic criteria as outlined in the DSM-5.
OCD is characterized by repetitive intrusive thoughts (obsessions) and/or behaviors that the person feels driven to perform (compulsions). The symptoms disrupt everyday life and cause significant levels of distress.
OCPD, on the other hand, is a type of personality disorder characterized by a generally lifelong pattern of continuous, habitual behaviors, rather than intrusive worries or distressing anxiety attacks. The defining features of OCPD are:
- Persistent and excessive concern with orderliness, perfectionism, and control. These concerns often come at the expense of flexibility, openness, and efficiency.
- The desire to keep things in control often leads to becoming overly occupied with details, rules, lists, order, organization, or schedules.
- The person may be excessively devoted to work and productivity, excluding leisure activities and friendships.
- Unlike OCD, those with OCPD often view their actions or habits as justified and are frequently unaware that the severity of their behaviors is problematic.