A cranial nerve nursing assessment is crucial for evaluating the neurological function of the twelve cranial nerves. It helps nurses identify early signs of dysfunction, make informed clinical decisions, and tailor patient-centered care plans.
Explore our comprehensive nursing guide to cranial nerve assessment – essential insights, procedures, and applications for holistic patient care.
A cranial nerve nursing assessment is crucial for evaluating the neurological function of the twelve cranial nerves. It helps nurses identify early signs of dysfunction, make informed clinical decisions, and tailor patient-centered care plans.
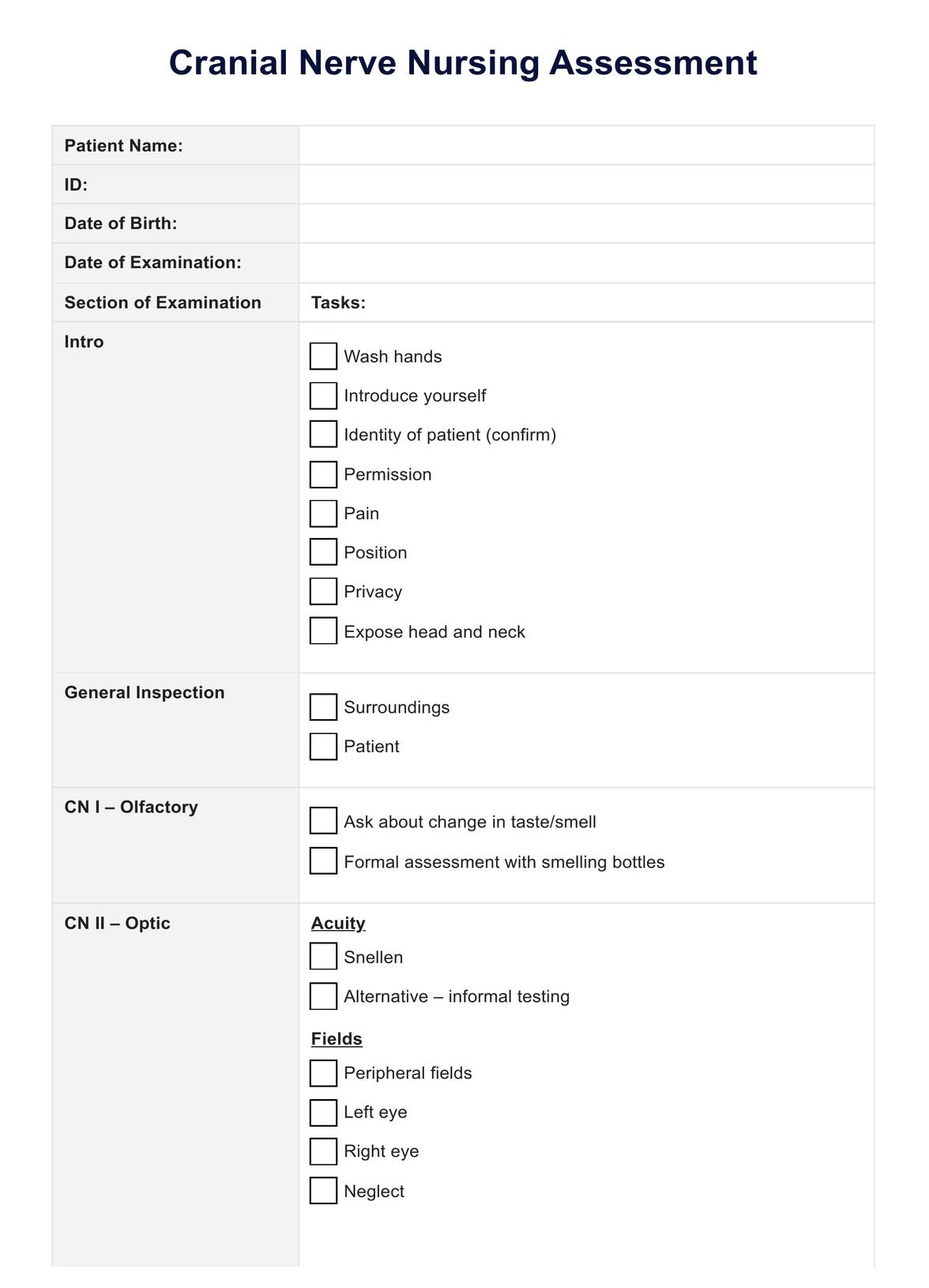
The assessment involves a systematic examination of each cranial nerve, assessing sensory and motor functions. Techniques include testing vision, hearing, facial movements, and evaluating reflexes. The goal is to identify abnormalities or deviations from expected responses.
A cranial nerve nursing assessment is essential in various clinical scenarios, including patients with head injuries, neurological disorders, or those undergoing surgeries affecting the cranial nerves. It is also valuable in assessing conditions such as strokes, facial paralysis, and sensory impairments.
EHR and practice management software
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments