No! As long as you thoroughly assess each cranial nerve, it does not matter what order you choose to complete the examination. Some would have learned the cranial nerves in order and so are used to using this order to structure the assessment. However, another approach is grouping cranial nerves by their function.
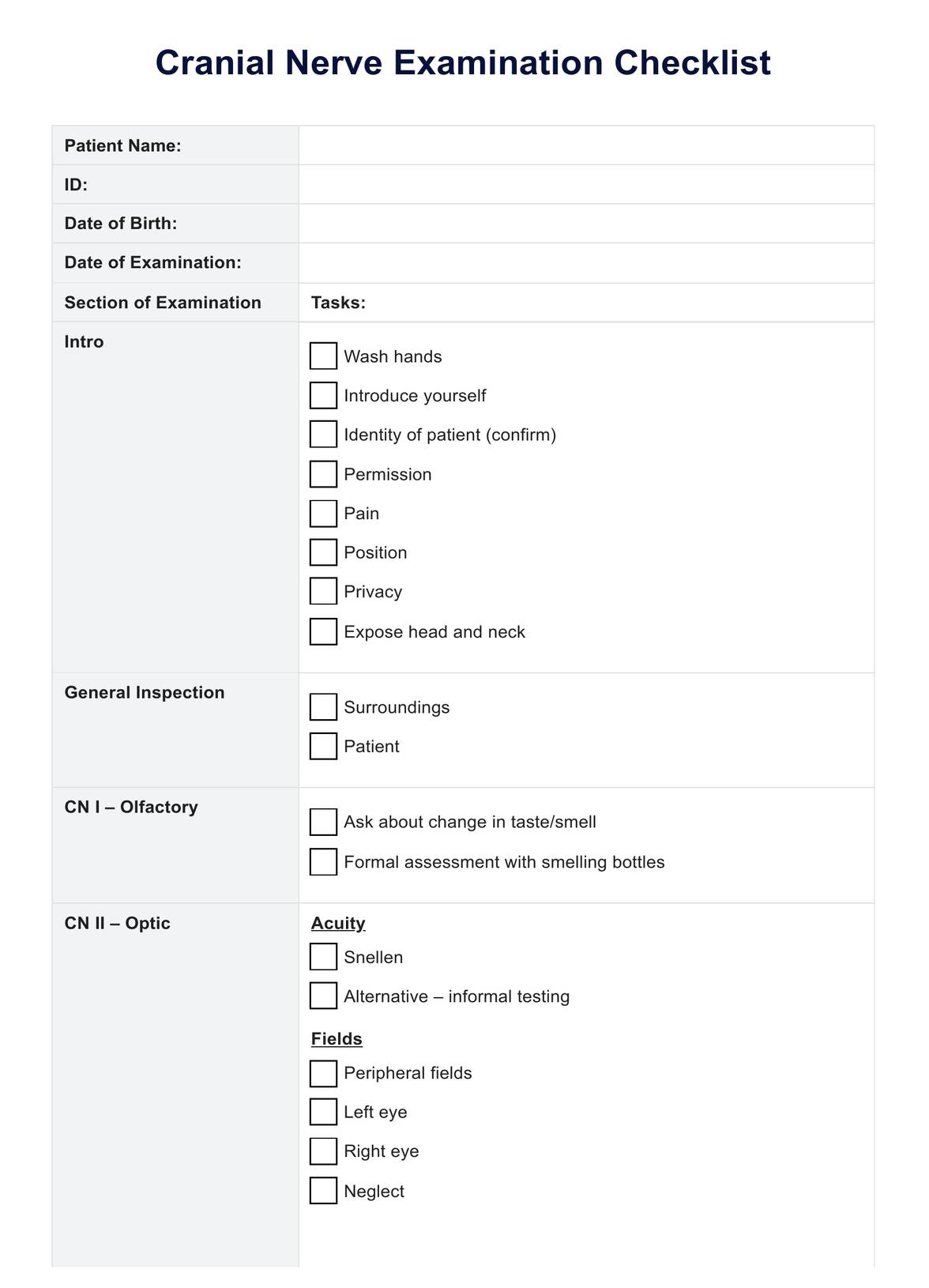
Cranial Nerve Examination Checklist
Perform your subsequent cranial nerve examination confidently using our concise and clearly formatted checklist.
Cranial Nerve Examination Checklist Template
Commonly asked questions
Similar to any clinical assessment, there may be some variability in your approach to evaluating each cranial nerve exam. However, certain aspects should consistently be maintained in every evaluation. These essential steps encompass acquiring the necessary tools, verifying the patient's name and date of birth, introducing yourself, articulating the examination in clear language, and obtaining consent before proceeding with the assessment.
Specific contraindications, such as facial trauma or swelling, can impede the accurate assessment of cranial nerves like CN III, IV, and VI. Despite technological advancements in imaging that have reduced the reliance on the results of a cranial nerve exam for diagnosing lesions, the examination remains a crucial component of the neurological assessment. It retains significance because it can be conducted swiftly with minimal equipment.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











