Trauma-informed approaches are frameworks that recognize the widespread impact of trauma on individuals and aim to create a safe and supportive environment for healing. These approaches prioritize understanding the effects of trauma on a person's mental, emotional, and physical well-being, emphasizing safety, trustworthiness, choice, collaboration, and empowerment.
Trauma-Informed Care Cheat Sheet
Unlock compassionate care with our Trauma-Informed Care Cheat Sheet—your essential guide to fostering healing and understanding in every interaction.
Trauma-Informed Care Cheat Sheet Template
Commonly asked questions
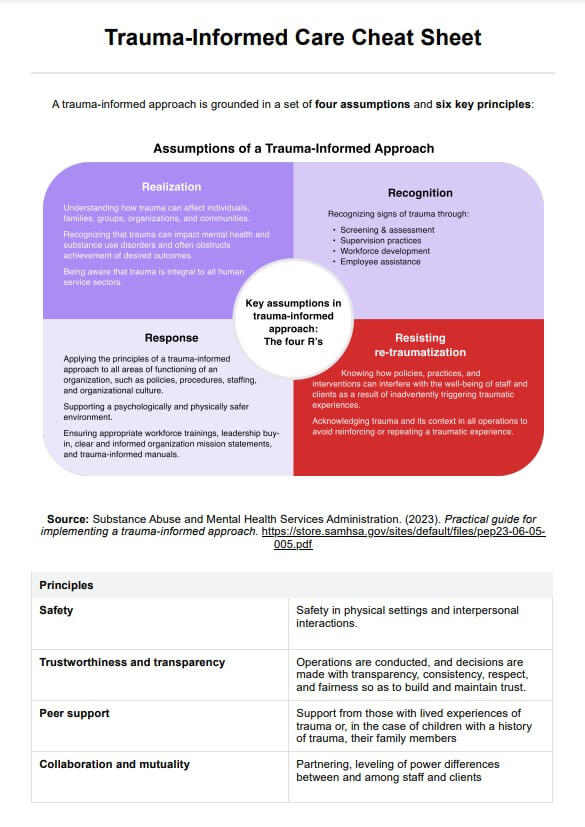
The 4 R's of trauma-informed care are 1) Realization of the widespread impact of trauma and its potential effects on individuals; 2) Recognition of the signs and symptoms of trauma in clients, families, and staff; 3) Response by integrating knowledge about trauma into policies, procedures, and practices; and 4) Resisting retraumatization.
The principles of trauma-informed care include safety, ensuring that clients feel physically and emotionally safe; trustworthiness, establishing transparency and consistency in practices; peer support, promoting mutual self-help and support among individuals; collaboration, involving clients in decision-making and care planning; empowerment, fostering a sense of control and choice; and cultural, historical, and gender considerations.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











