A comprehensive Mental Health Assessment gathers information about the client's presenting problems, mental health history, medical history, family history, substance use, safety concerns, and treatment goals. It may involve standardized screening tools, a mental status exam, and a diagnostic interview.
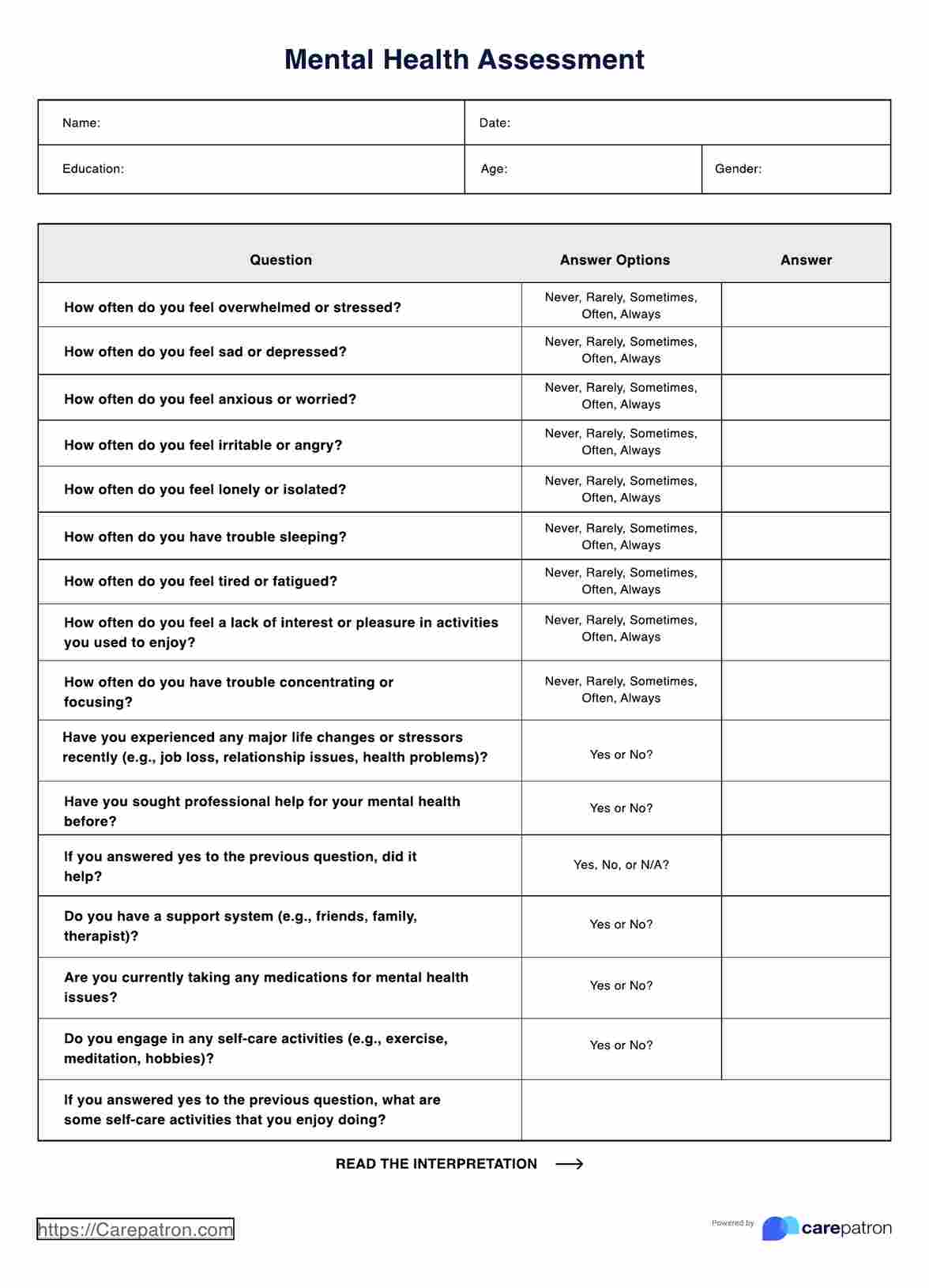
Mental Health Assessment
Discover how to use a mental health assessment with our guide. Includes a sample template, interpretation, FAQs, and benefits of using a free assessment.
Mental Health Assessment Template
Commonly asked questions
When documenting a Mental Health Assessment, you can use a structured SOAP note format that includes the Subjective section to record the client's self-reported symptoms, concerns, and goals in their own words; the Objective section to document observable signs and behaviors during the assessment; the Assessment section to provide your clinical impressions; and the Plan section to outline the recommended treatment approach.
The time required to complete a Mental Health Assessment can vary depending on the setting and the client's specific needs. A thorough initial assessment may take 30-60 minutes or longer. Follow-up assessments are typically shorter and focus on monitoring progress and adjusting the treatment plan.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











