Anyone can develop an eating disorder, regardless of age, sex, racial or ethnic background. However, teenagers and young women are often more vulnerable due to various biological, social, and psychological factors.
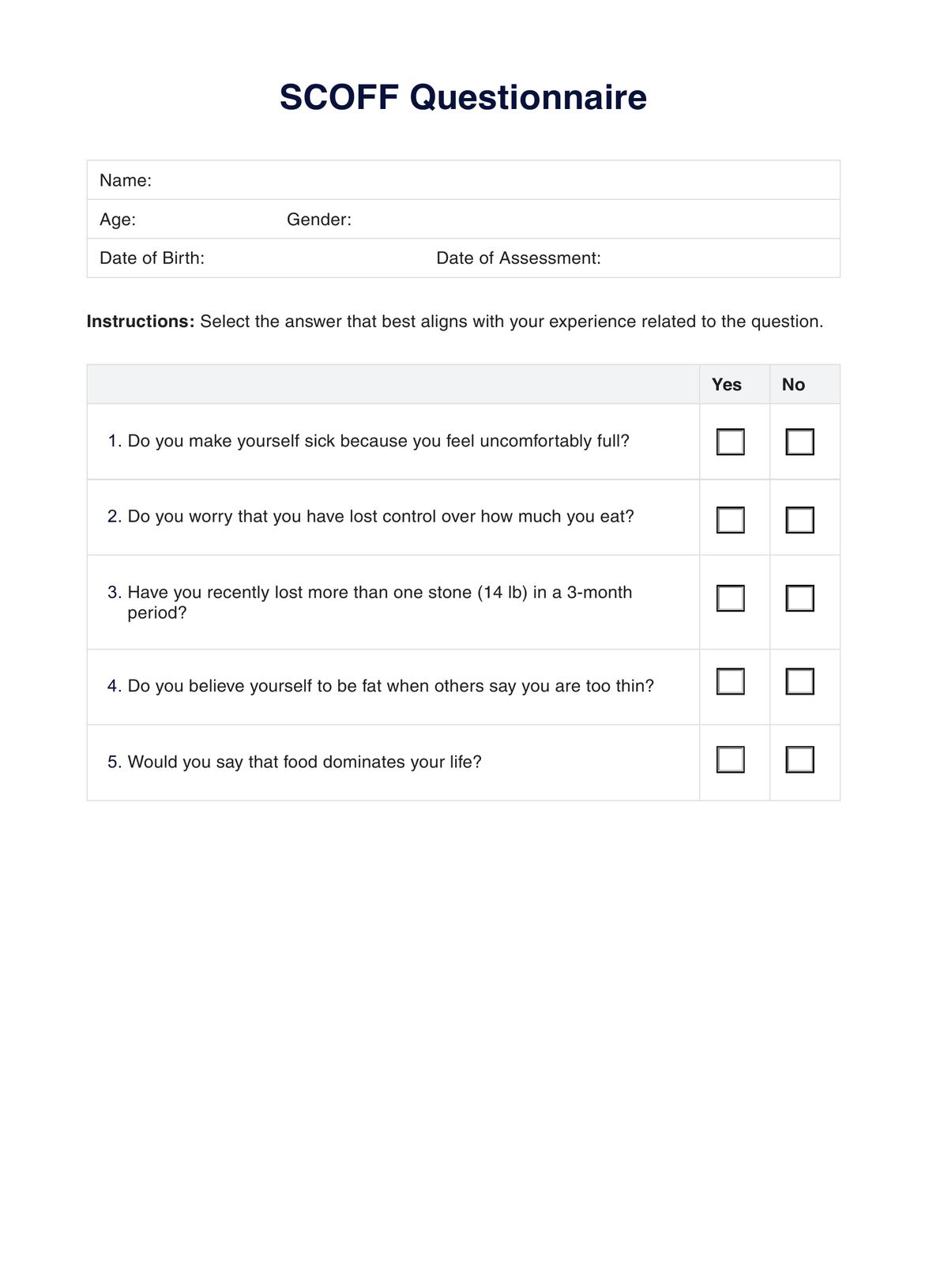
SCOFF Questionnaire
Explore using the SCOFF Questionnaire to detect disordered eating symptoms and plan for early intervention. Download a free PDF resource here.
SCOFF Questionnaire Template
Commonly asked questions
Signs may include extreme preoccupation with weight and food, drastic changes in eating habits, excessive exercise, withdrawal from social activities, and significant weight changes. Emotional signs include distress, guilt, or shame about eating habits.
Start by talking to a healthcare provider, such as a doctor or mental health professional, who can provide referrals to specialists in eating disorders. There are also helplines, websites, and support groups that offer resources and support for those affected by eating disorders and their loved ones.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











