Critical questions for depression assessment include inquiries about mood, interest in activities, sleep patterns, appetite, energy levels, and thoughts of self-harm.
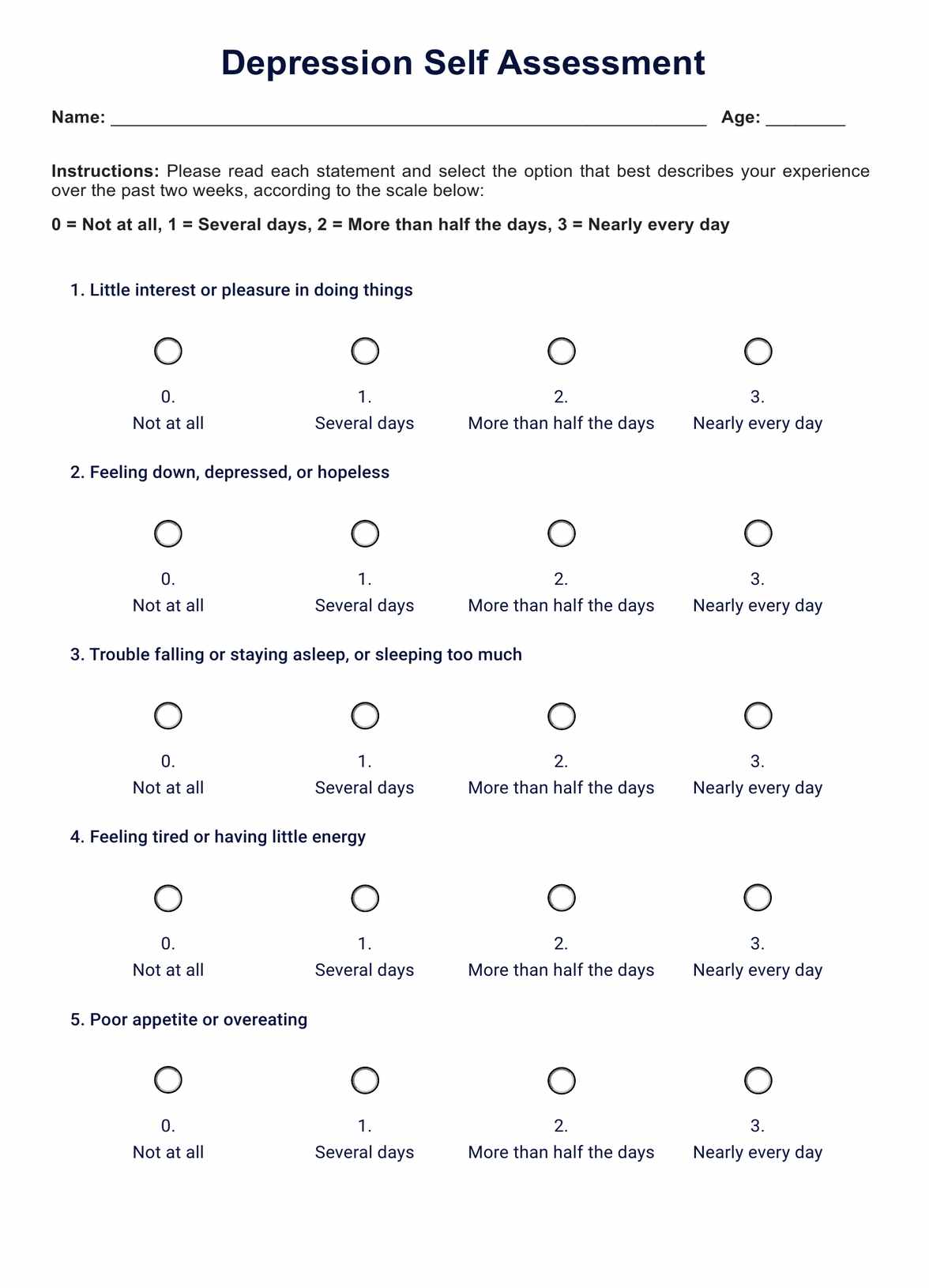
Depression Self-Assessment
Explore our comprehensive guide on the Depression Self-Assessment, designed for mental health professionals to evaluate and manage depression effectively.
Use Template
Depression Self-Assessment Template
Commonly asked questions
Depression often leads to reduced social interaction, trouble falling or staying asleep, poor appetite, difficulty focusing, and diminished motivation.
Depression can change how a person feels and behaves, often resulting in increased sadness, withdrawal, and a negative outlook, but it doesn't permanently alter personality.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











