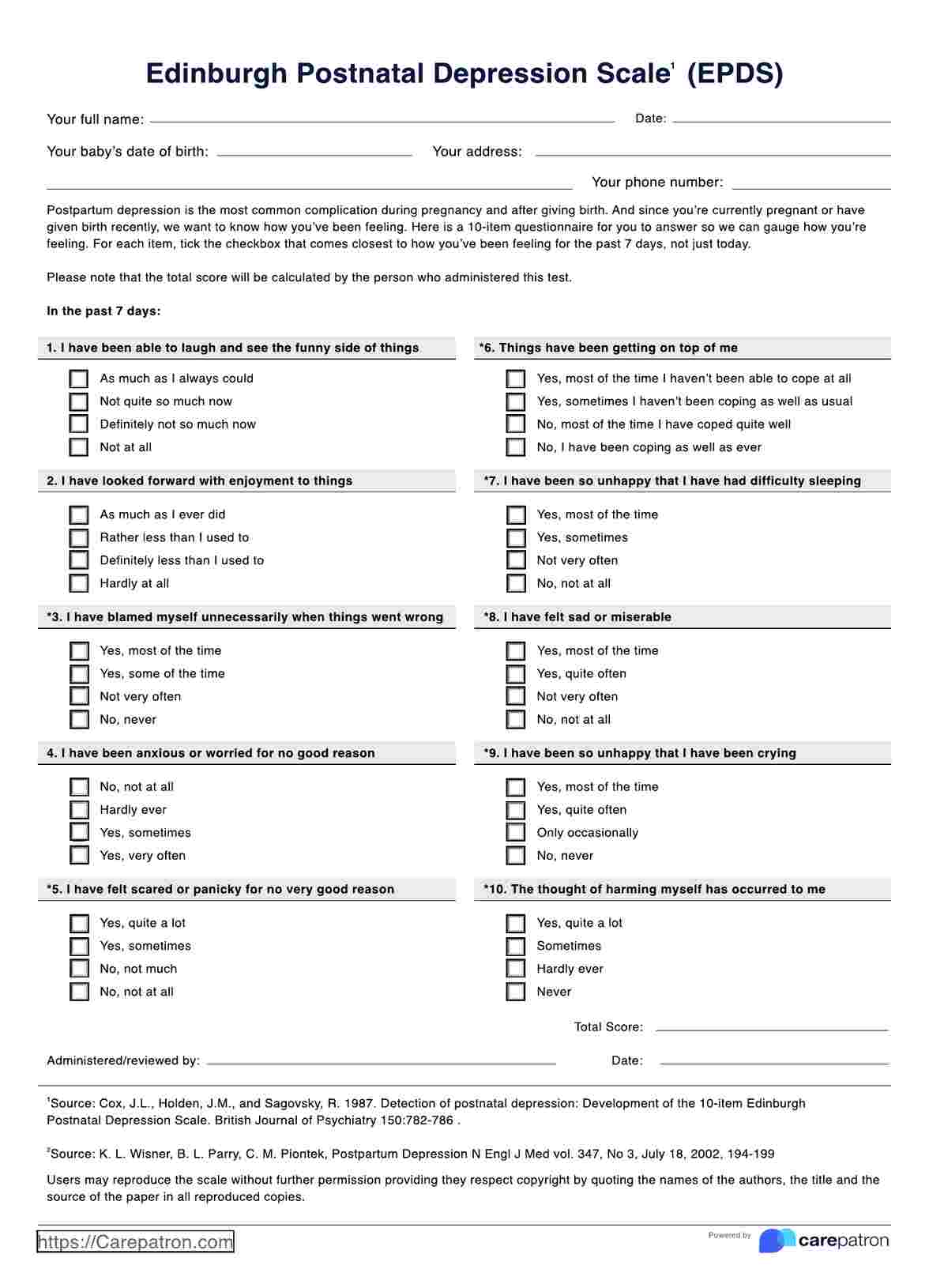
The Edinburgh Postnatal Depression Scale (EPDS) is a 10-item self-report questionnaire used to screen for symptoms of postnatal depression in new mothers. It helps healthcare professionals identify emotional and psychological distress that may develop after childbirth. Each item is scored on a scale of 0 to 3, reflecting how the mother has felt during the previous seven days.
Edinburgh Postnatal Depression Scale (EPDS)
Use the Edinburgh Postnatal Depression Scale (EPDS) to help you assess depression among mothers. Download the free template now.
Edinburgh Postnatal Depression Scale (EPDS) Template
Commonly asked questions
A normal EPDS score typically ranges from 0 to 9, suggesting no or minimal signs of depression. Scores between 10 and 12 indicate possible mild depression and warrant further observation. A score of 13 or higher suggests a high likelihood of postpartum depression and should prompt a comprehensive clinical assessment.
The EPDS measures the intensity of depressive symptoms such as sadness, anxiety, guilt, and sleep or appetite changes in postpartum individuals. It focuses on emotional and cognitive symptoms rather than physical ones, making it suitable for distinguishing depression from normal postnatal fatigue. Its main goal is early detection to enable timely intervention and support for maternal mental health.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











