The Beck Depression Inventory (BDI) and Beck Depression Inventory-II (BDI-II) are both self-report measures of depression, but the BDI-II is an updated version that better aligns with the diagnostic criteria for depression in the Diagnostic and Statistical Manual of Mental Disorders. The BDI-II also uses a 2-week time frame, compared to the 1-week time frame of the BDI, and has updated language and response options to improve clarity and relevance.
Beck Depression Inventory
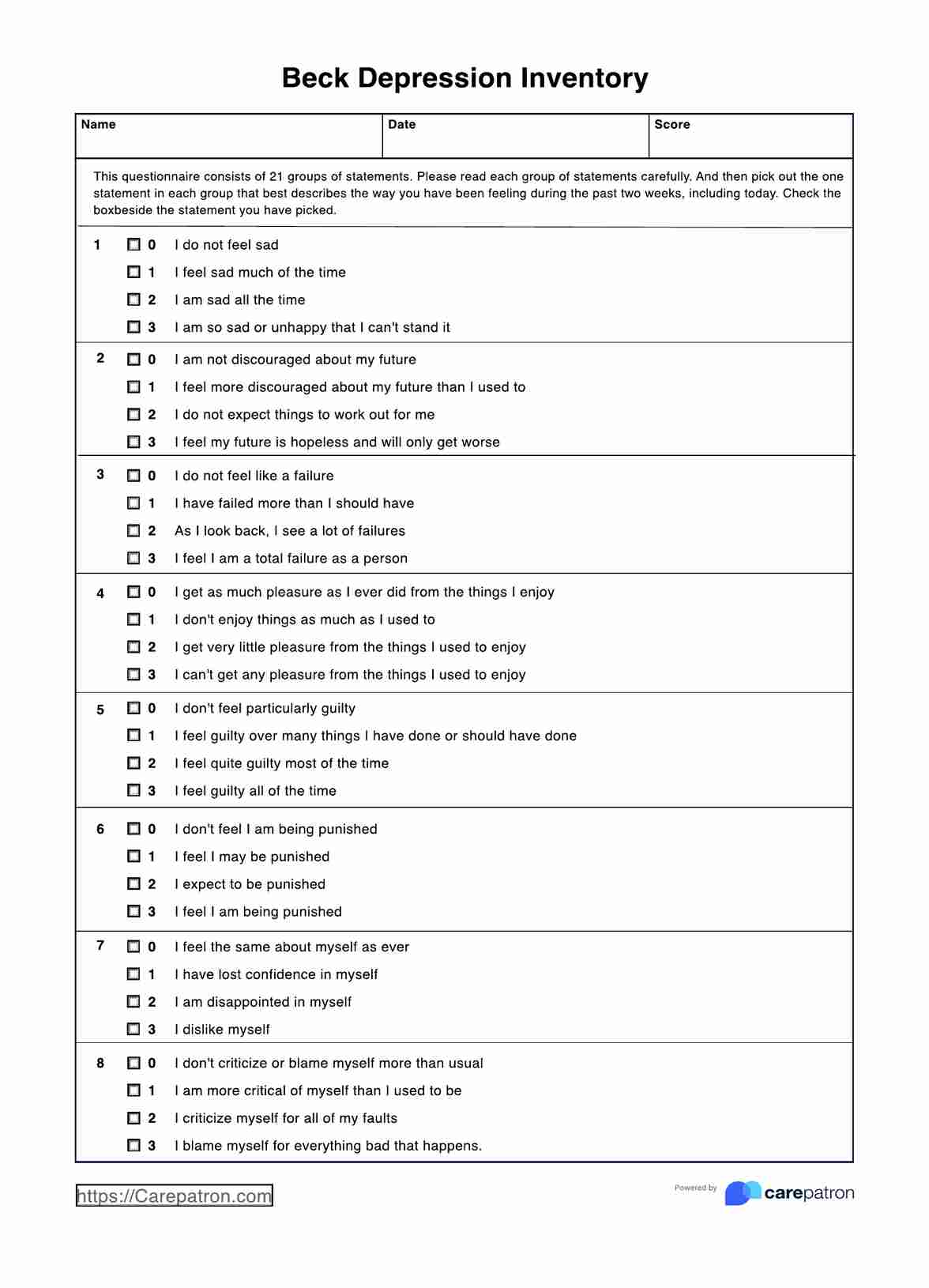
Utilize Beck's Depression Inventory to gauge depressive symptoms effectively. Download our free PDF for professional assessment and insight.
Beck Depression Inventory Template
Commonly asked questions
The Beck Depression Inventory (BDI is scored on a scale from 0 to 63, with higher scores indicating more severe depressive symptoms. Scores are typically interpreted as follows: 0-13 (minimal depression), 14-19 (mild depression), 20-28 (moderate depression), and 29-63 (severe depression). The BDI is designed to assess the severity of depression symptoms over the past two weeks.
The Beck Depression Inventory-II (BDI-II) is designed for individuals aged 13 and older, including adolescents and adults. It can be used to assess depression in various populations, including clinical and non-clinical samples.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











