Postpartum Care Plans provide structured emotional support by including resources for mental health care, such as counseling and support groups. They also help mothers manage stress by organizing a support system for daily responsibilities, promoting overall mental wellness.
Postpartum Care Plan
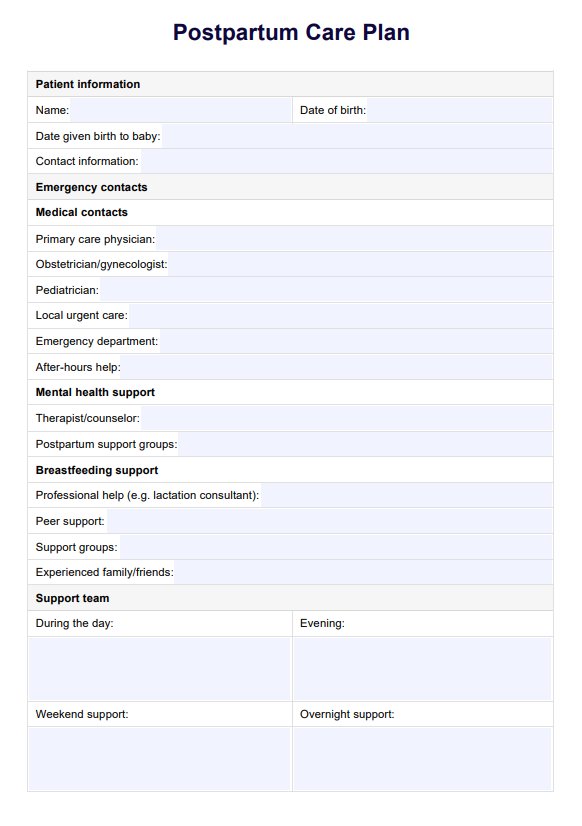
Download our free Postpartum Care Plan PDF to guide new mothers through recovery and ensure optimal postnatal health.
Use Template
Postpartum Care Plan Template
Commonly asked questions
A Postpartum Care Plan ensures that both mother and baby are supported by addressing breastfeeding, pediatric visits, and other newborn care essentials. It also guides the coordination of care between the mother and her postpartum care team to optimize infant health outcomes.
They can use care plans to identify and address postpartum complications and risks through accurate nursing diagnosis and intervention.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











